Chair's Message Archive - 2021
November 2021
Anatomic Pathology Updates
We are delighted to announce our new Director of Surgical Pathology, Dr. Gregory Gates. In this role, Dr. Gates will be responsible for overseeing the operation of the Division of Anatomic Pathology, which includes the following services: Autopsy, Cytopathology, Surgical Pathology, Hematopathology, Molecular Pathology, Cytogenetics, and Neuropathology. Dr. Gates will continue in his current role as the Director of Immunohistochemistry lab. Please join us in congratulating Dr. Gates and we look forward to his leadership in this important role!
Clinical Pathology Updates
The Division of Microbiology under the direction of by Dr. Omai Garner, not only plays an essential role in patient care, but also is continuously collaborating with UCLA Infection Prevention to prevent healthcare associated infections. In July 2021, the UCLA Infection Prevention team noticed a cluster of bacteremia cases with Burkholderia cepacia complex (BCC), a group of environmental Gram-negative bacteria that are frequently associated with nosocomial infection. Coincidentally, several institutions across the nation also reported an unusual increase of BCC bacteremia cases. Through active communication with other clinical microbiology laboratories, the UCLA Clinical Microbiology lab directors, Drs. Garner, Shaun Yang and Suki Chandrasekaran, learned that ultrasound gel used prior to intravenous catheter insertion was suspected as the source of the bacteria. Using microbial whole-genome sequencing (WGS), the bacteria isolates were quickly characterized. Furthermore, our Clinical Microbiology lab provided high-resolution genetic information and revealed that these bacteria, along with the bacteria isolated from other institutions, were essentially identical; the bacteria were identified as Burkholderia stabilis, indicating a nation-wide outbreak with the same source of contamination. In the meantime, culture of samples from the ultrasound gel grew the same bacteria as proven by WGS. Based on definitive information generated by our microbiology lab, Infection Prevention immediately replaced the ultrasound gel with another vendor’s product at all clinical locations throughout UCLA Health. No new B. stabilis bacteremia has occurred since cessation of the brand of ultrasound gel associated with the contamination. The astute investigation and collaboration between the UCLA Clinical Microbiology Laboratory and the Infection Prevention team quickly identified the source and contained the outbreak in less than one month. This case, as well as many others, demonstrate the value of the robust microbial genomic surveillance system that the UCLA Clinical Microbiology lab has established by using WGS to assist in outbreak investigation in real-time.
Additionally, we are pleased to announce our Faculty and Department made the decision to change the Clinical Pathology Division’s name to Laboratory Medicine to accurately reflect their activities.
Immunogenetics Updates
Clinical
The UCLA Immunogenetics Center (UIC)IC provided Histocompatibility and Immunogenetics testing for 790 solid organ transplants for the 5 transplant centers we serve (UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange) and performed Histocompatibility testing for 25 kidney paired donations at UCLA. UIC established new partnerships with USC, Loma Linda, Cedars Sinai and Children’s Hospital Los Angeles to provide crossmatch testing to support the new United Network for Organ Sharing kidney transplant allocation policy.
UIC successfully completed several strategic Information Technology Projects. A major goal was to build the UC Davis electronic medical record with historical donor and recipient transplant information prior to 2019. This project called the “UC Davis Historic Load” was completed in a comprehensive electronic record of all of UC Davis’s transplant patient data. This will greatly enhance patient care and clinical research. UIC has also validated and deployed new workflows and processes to improve efficiencies for EPIC and Beaker billing. Another major accomplishment was establishing electronic reporting of deceased donor HLA typing from UIC Histotrac to One Legacy OPO Digital Donor. Recent changes in United Network for Organ Sharing policies required UIC to establish order/reporting and sample storage workflow for 10-year Storage of Living Donor Samples in accordance with UNOS Policy Change. Another major accomplishment was the implementation of the MediaLab document control system in August of 2021.
UIC welcomes Amy Ramirez, Client Services Supervisor and Dr. Rebecca Sosa, Health Sciences Assistant Professor to our team.
Quality
UIC continues to build upon its quality program. Five major quality projects were implemented and completed including:
- UIC performed a comprehensive review and Dr. Hickey established a new protocol with UCLA Compliance to ensure restriction of immunogenetics tests from patient portal or release.
- In collaboration with the Digestive Disease team led by Guy Weiss, MD, UIC faculty developed new Celiac Genotype Interpretative Comments based on a comprehensive review of the literature and revision to align with clinical application.
- Dr. Cappelletti and Mary Alice Mita established protocols for inpatient and outpatient draws of healthy control donors, as well as local healthy donor pool for Immune Assessment Core tests.
- UIC Faculty led by Dr. Yuxin Yin and supervisor Ping Ge performed validation of Robosep automated Cell Isolation and trained 65 staff.
- Dr. Hickey instituted the UCLA Department of Pathology Resident Lecture Series entitled “Department of Pathology and Laboratory Medicine Quality Program” with the goal of educating the next generation of pathologists in quality of medicine and health care.
Education
The UIC educational program led by Jennifer Zhang, Ph.D., leveraged the zoom platform to expand training in Immunogenetics and Histocompatibility testing to our partner institutions. The faculty taught 5 educational lecture series consisting of 6 seminars to pathology residents, pathology fellows, transfusion medicine fellows, clinicians and transplant coordinators at UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange, One Legacy, and Kaiser Permanente Southern California.
Research
UIC faculty and fellows published 21 publications and Dr. Elaine Reed was awarded 1 new NIH grant. Dr. Reed received a philanthropic grant donation from an Aestiva Software Founder, to establish a post-doctoral research fellowship focused on understanding mechanisms of antibody mediated heart transplant rejection.
UIC welcomes Meagan Jenkins, PhD joined the Reed Lab as new Postdoctoral Scholar. Her research is aimed at understanding cellular immunity to SARS-CoV-2 and correlates of immune protection.
UIC serves as CAP proficiency test provider since 2003 and has provided educational and proficiency testing programs to the Immunogenetics Community for 47 years. Given the recent interest in non-classical HLA genes in transplantation and disease association the UCLA Cell Exchange program added analysis and reporting of non-traditional HLA loci (HLA-E, -F, -G, -H, MICB) to the DNA Exchange proficiency test program.
October 2021
The Department continues to take an active role in training outstanding pathologist-scientists. In association with the UCLA-STAR program, we have created a training pathway tailored to the unique needs of pathologist-scientists. One of our residents, Jennifer Chia, MD, PhD, entered this pathway when she began her AP residency in 2018. Dr. Chia is currently a hematopathology fellow in our program, having completed her AP training in June 2021, which included a research block in the laboratory of Dr. Alex Hoffmann, the Director of the Institute for Quantitative and Computational Biosciences. During this research block, Dr. Chia developed extensive preliminary data for a highly innovative project. Her research combines her training in hematopathology and her interest in computational biology to study the role of the NF-kappa B transcription factor in myeloid proliferations. Her work will set the stage for important scientific discoveries during a dedicated research phase as a STAR fellow and provide the practical experience and mentoring for an independent research program in the years to come.

Dr. Jennifer Chia
The UCLA-Caltech Medical Scientist Training Program (MSTP) is a flagship education program in the David Geffen School of Medicine. The UCLA-Caltech MSTP offers students rigorous combined MD/PhD training across disciplines relevant to human health and medicine, ranging from basic sciences to translational research to engineering to social sciences and health policy. The program’s success is predicated on the breadth of opportunities and excellence of research at UCLA. In addition, select individuals pursue research at Caltech through an institutional partnership established two decades ago. The MSTP recruits and supports students of diverse backgrounds and experiences, seeking individuals with a passion for scientific knowledge and a life-long commitment to research and leadership in medicine. There are currently 113 students enrolled in the UCLA-Caltech MSTP making it one of the largest and most diverse in the country. Students have a longstanding record of accomplishment, typically securing extramural NIH or other private foundation funding for their PhD training and averaging six authored papers (including 2+ as first author and a best first author paper in journals with an average impact factor of 14)! Graduates match in the most competitive residency programs across the country, while more than 70% of alumni remain in academia after completing their postgraduate training. Notable alumni include several current UCLA Department of Pathology and Laboratory Medicine faculty, including Drs. Michael Teitell, Jonathan Zuckerman, and Valerie Arboleda.
Dr. David Dawson
Pathology faculty are heavily involved in the UCLA-Caltech MSTP through participation in program admissions, research mentorship, and leadership. Many MSTP students pursue their PhDs in pathology research laboratories with pathology faculty serving as primary PhD advisors or thesis committee members. Pathology is by far the most heavily represented department on the MSTP Admissions Committee, which currently includes Drs. Valerie Arboleda, Gay Crooks, David Dawson, Dinesh Rao, Peter Tontonoz, Harry Vinters, and Michael Teitell. Dr. Teitell recently served as an MSTP Associate Director from 2013-2019, stepping down when he became Director of the Cancer Center. Previously the Associate Director for Admissions and Mentorship (2015-2019), Dr. David Dawson became co-Director of the MSTP in January 2020, a primary leadership role that is shared co-equally with a second co-Director, originally Dr. Carlos Portera-Cailliau (Dept. of Neurology) and more recently Dr. Olujimi Ajijola (Dept. of Medicine).
September 2021
We are pleased to feature the curriculum redesign within DGSOM and medical and dental curriculum updates.
DGSOM has undergone a major curriculum redesign, the intent of which is to “empower students to become physicians committed to excellence and leaders in innovation, research, health, education, advocacy and humanistic care.” As the new curriculum emphasizes self-regulated learning, whereby the learners diagnose needs, formulate goals, identify resources, implement appropriate activities, and evaluate outcomes, it is a bit different from the “rote learning” based curriculum previously used to train physicians.
As a result of the new curriculum implementation, the inaugural class of 2025 will spend roughly one year learning basic science, doctoring, and clinical skills/reasoning before beginning their core clinical clerkships during the second year of training. The learners will then embark on a “discovery year,” a period of time during which they will be able to either immerse themselves into specific areas of focus within a variety of arenas (i.e. research, innovation, advocacy, etc.) or pursue a dual degree at UCLA. Additionally, the new curriculum contains “themes” that focus on Structural Racism/Health Equity, Medical/Health Humanities, and Ethics, all of which will be integrated throughout the entire four years of training. This is truly an exciting time for medical education! For more details regarding the new medical school curriculum, please read more here.
Last year, as part of the curriculum revision for the School of Dentistry (SOD) and in response to a fundamental change in the National Dental Board examination, the SOD approved changes related to our gross anatomy course. In brief, additional anatomy dissections and several anatomy reviews were added to the curriculum, and anatomy courses were rearranged in time so to create more thematic integration across the curriculum. The ultimate goal of these changes is to help students better learn the material, prepare for board exams and ultimately become successful dentists.
In total over 30 faculty in our Department contribute to our DGSOM and SOD curricula. We are grateful for your effort, dedication, and enthusiasm in providing our dental and medical students with an excellent education.
August 2021
We are pleased to announce a successful launch of Pathology Grand Rounds. Throughout the year, this series will include Clinical Seminar Series (currently known as the Visiting Professor Series), Research Seminar Series, as well as Daljit S. & Elaine Sarkaria/Quality Day, Lya & Harrison Latta, and Walford Lectureships. Our named lectureships will be advertised as the named lecture, as part of Pathology Grand Rounds. The goal of the rebranding is to gain increased visibility for our internal and external audiences as well as enhance opportunities for sponsorship of invited speakers among multiple different areas of our Department. Grand Rounds will take place on the 2nd and 4th Friday of the month from 8:00 AM-9:00 AM and/or 12:00 PM-1:00 PM.
We are excited to announce our speaker selection for 2021-2022 Pathology Grand Rounds. Our first presentation took place on Friday, July 23rd with Dr. Peter Hotez, Professor of Pediatrics and Molecular Virology & Microbiology at Baylor College of Medicine, speaking on "COVID-19 Vaccines: Science vs. Antiscience.” We were thrilled to host such a prominent figure in his field.
We also thank our Department Inclusive Excellence committee for their future work toward increasing the diversity in the invited speakers. With the creation of the Department Grand Rounds series, that encompasses previously discreet invited lectures, we have better opportunities to diversify the entire group of outside speakers.
The full speaker schedule is now available on our website.
July 2021
As we begin the new academic year, I would like to provide a warm welcome to our new Residents, Fellows, and Faculty. Additionally, I would like to highlight the Farewell Ceremony awards and recipients. We wish our graduating Trainees the best in their future endeavors. I am also pleased to announce the launch of our Wellness pages and resources available on our website.
Please join me in welcoming our new PGY1 Residents!

Taylor Howard
University of Nevada SOM

Andrea Oliveira-Kowaleski
Universidade Federal de Sao Carlos, Brazil

Joshua Pierce
University of Texas Southwestern Medical School at Dallas

Rakshit Tyagi
State University of New York Upstate Medical University

Alexandria Wellman
Southern Illinois University SOM

Amanda Zand
University of Missouri, Columbia SOM
Please join me in welcoming our new ACGME Fellows, Non-ACGME Fellows, and Clinical Post Docs!
Jennifer Chia, MD, PhD
Medical School – Weill Cornell Medicine of Cornell University
Residency – University of California, Los Angeles
Hematopathology
Rina Eden, DO
Medical School – Western University of Health Sciences: College of Osteopathic Medicine of the Pacific
Residency – San Antonio Military Medical Center
Transfusion Medicine
Karam Han, MD
Medical School – Boston University SOM
Residency – Case Western Reserve University/Metrohealth Medical Center
Neuropathology
Alden Huang, PhD
PhD – University of California, Los Angeles
Laboratory Genetics & Genomics
Lawrence Kuklinski, MD
Medical School – Dartmouth Geisel SOM
Residency – University of California, Los Angeles – Dermatology
Dermatopathology
Katy Lawson, MD
Medical School – Oregon Health and Science University
Residency – University of California, Los Angeles
Hematopathology
Christine Lee, MD
Medical School – Tulane University School of Medicine
Residency – University of California, Los Angeles
Dermatopathology
Ami Mon, MD
Medical School – St. George's University SOM
Residency – University of Hawaii
Fellowship – Pediatric Pathology – Baylor College of Medicine
Cytopathology
Rugved Pattarkine, MD
Medical School – Smolensk State Medical University
Residency – New York Medical College/Westchester Medical Center
Transfusion Medicine
Reiri Sono, MD
Medical School – Indiana University SOM
Residency – Mount Sinai Hospital
Fellowship – University of California, San Francisco – Clinical Informatics
Molecular Genetic Pathology
Kevin Van Smaalen, MD
Medical School – Loma Linda University SOM
Residency – Emory University SOM
Cytopathology
Charisse L. Treece, MD
Medical School – University of the East Ramon Magsaysay Memorial Medical Center, Quezon City, Philippines
Residency – Anatomic and Clinical Pathology, University of Illinois at Chicago, Chicago, IL
Surigical Pathology Fellowship/Clincial Informatics
Cameron Wales, MD
Medical School – University of Central Florida SOM
Residency – University of California, San Diego
Dermatopathology
Non-ACGME Fellows
Zhengshan Chen, MD, PhD
Medical School – Peking University Health Science Center
Residency – University of Southern California
Fellowship – University of Chicago – Visiting Student University of California, San Francisco Postdoctor
Surgical Pathology Fellowship/General Surgical Pathology
Yipeng Geng, MD, PhD
PhD – Vanderbilt University
Medical School – Sun Yat-Sen University
Residency – University of California, Los Angeles
Fellowship – Visiting Scholar – Lehigh Valley Hospital
GI/Liver Pathology Fellowship
Mahdi Khoshchehreh, MD, MS
MS – Applied Epidemiology and Biostatistics, University of Southern California
Medical School – Tehran University of Medical Science, Tehran
Residency – University of Southern California, LAC+ USC Medical Center
Fellowship – Surgical Pathology Fellow OVMC – University of California, Los Angeles
Surgical Pathology Fellowship/Women's Health
Trang Lollie, MD
Medical School – Tulane University School of Medicine
Residency – University of California, Los Angeles
GI/Liver Pathology Fellowship
Daniel Manzoor, MD
Medical School – St. George's University School of Medicine, Grenada, West Indies
Residency – Pathology, Anatomic/Clinical, Cedars-Sinai Medical Center
Surgical Pathology Fellowship/General Surgical Pathology
Aidas J. Mattis, MD, PhD
Medical School & PhD – University of Illinois, Urbana-Champaign
Residency – Barnes-Jewish Hospital, Washington University, St. Louis, MO
Fellowship – Medical Renal Pathology, Cedars-Sinai Hospital, Los Angeles
Surgical Pathology Fellowship/OVMC
Manando Nakasaki, MD, PhD
PhD – Graduate School of Medicine Osaka University
Medical School – Osaka University Medical School
Residency – Department of Pathology, University of California, Irvine
Surgical Pathology Fellowship/Bone and Soft Tissue
Dandan Wang, MD
Medical School & Residency – Zhongshan Ophthalmic Center, China – LAC + USC Medical Center
Research Fellowship – University of California, San Francisco
Clinical Instructor – University of Southern California
Intern – University of Nevada, Reno
Surgical Pathology Fellowship/Women's Health
Clinical Post Docs
Stacey Ceron, PhD
PhD – Dartmouth College
Clincial Microbiology
June Chan, PhD
PhD – Johns Hopkins Bloomberg School of Public Health
Clincial Microbiology
Sun-Mi Choi, MD, PhD
PhD – Louisiana State University School of Medicine
Immunogenetics
It is with great pleasure I announce our incoming faculty joining the department. Please join me in welcoming Dr. Lin, Dr. Erika Rodriguez, Dr. Fausto Rodriguez, and Dr. Sosa!
Fumin Lin received his Ph.D. from Duke University in 2011. He completed his postdoctoral training in National Institute of Environmental Health Sciences and Baylor College of Medicine. In 2015, he joined the Division of Genomic Diagnostics at the Children’s Hospital of Philadelphia (CHOP), where he contributed to the clinical case analysis and assay development for cancer molecular tests, SNP array and constitutional exome as a clinical genomic scientist. He was accepted by the Laboratory Genetics and Genomics Fellowship Program at CHOP in 2018 and will complete the training in June 2021. His research interests lie in understanding the molecular mechanisms in various malignancies and utilizing mutation signatures in cancer diagnosis. He enjoys playing basketball and table tennis in his spare time.
We are delighted to welcome Dr. Fumin Lin in his new role as Assistant Clinical Professor in the Molecular Diagnostic Section in the Division of Anatomic Pathology. Dr. Lin will be signing out Cytogenetic and Molecular cases, as well as participating in all activities of both areas.
Erika Rodriguez received her M.D. from the Federal University of Sergipe (UFS), Brazil, and her Ph.D. from the University of Sao Paulo Medical School where she also completed her anatomic pathology residency training. She then moved to the Mayo Clinic in 2007 where she started her AP/CP residency training. She joined the faculty of Johns Hopkins Hospital in 2014 after undergoing fellowship training in Cytopathology (University of Pittsburgh) and Surgical Pathology (University of Pennsylvania). She has worked predominantly in the Division of Cytopathology, where she recently led the implementation of EPIC Beaker. She is serving currently as the Director of Anatomic Pathology at Bayview Medical Center, Johns Hopkins. Her academic interests are broad with the topics of health disparities, quality and pulmonary pathology being close to her heart. Her favorite things to do are playing with her daughters, Pilates, yoga, reading and walking on the beach. We are delighted to welcome Dr. Erika Rodriguez to the UCLA Department of Pathology and Laboratory Medicine in her new role as Associate Clinical Professor serving the Cytology and General Surgical Pathology specialties.
Dr. Fausto J. Rodriguez is currently professor of pathology, oncology and ophthalmology and molecular genetic pathology fellow at the Johns Hopkins University School of Medicine. Dr. Rodriguez completed training in anatomic pathology and neuropathology at Mayo Clinic, Rochester, MN, followed by a neuro-oncology research fellowship under a T32 training grant. After serving as senior associate consultant for two years, he moved to Hopkins in 2010 and has been director of the clinical (surgical) neuropathology service for the past 5 years. His clinical and research work aims to identify diagnostic, prognostic, and therapeutic biomarkers and targets in tumors of the central and peripheral nervous system, particularly those that develop in young patients and in the context of inherited tumor syndromes.
We are delighted to welcome Dr. Fausto Rodriguez to UCLA Department of Pathology and Laboratory Medicine in his new role as Chief of Neuropathology and Professor. Additionally, he will serve as Neuropathology Fellowship Director and as the Director of the Pathology Core for Brain SPORE. As Director, he will oversee all activities within the Division of Neuropathology, including clinical, research and education.
Dr. Rebecca Sosa earned her PhD in Cell and Molecular Biology at the University of Texas at San Antonio where she studied the role of cytokines in autoimmune disease of the central nervous system including multiple sclerosis and experimental autoimmune encephalomyelitis. For her postdoctoral training, she moved to the laboratory of Dr. Elaine Reed, in the Department of Pathology and Laboratory Medicine, University of California, Los Angeles, where her work focused on understanding the interplay between the innate and adaptive immune system in ischemia reperfusion injury in human liver transplantation. In June 2021, Dr. Sosa successfully completed the Immunogenetics and Histocompatibility Laboratory Director Fellowship Program at the UCLA Immunogenetics Center.
In July 2021, we welcome Dr. Rebecca Sosa in her new role as an Assistant Laboratory Director, and Health Sciences Assistant Clinical Professor in the UCLA Immunogenetics Center, Department of Pathology and Laboratory Medicine. In this role, Dr. Sosa will be responsible for technical oversight of immunogenetics and histocompatibility testing, reviewing and signing out test results, clinical consultation, teaching and creative contributions.
Please join me in honoring our Farewell Ceremony award recipients and graduating Trainees!
Justine Pomakian Memorial Award – Shih-Mao Teng
Inaugural Maryam Sayah Memorial Award – Robin Dietz Jr., MD
Housestaff Recognition Awards – Awarded by our Pathology Residents
Faculty Teaching Award in Anatomic Pathology – Jeffrey Krane, MD, PhD
Faculty Teaching Award in Clinical Pathology – Niroshi Senaratne, PhD
Anatomic Pathology Technical Staff Award – Jessica Jones
Clinical Pathology Technical Staff Award – Shih-Mao Teng
Administrative Staff Appreciation Award – Veronica Mani
Department Years of Service
5 Years of Service
Jeffrey Goldstein, MD
Andrea McGonigle, MD
10 Years of Service
Hanlin Wang, MD
15 Years of Service
Neda Moatamed, MD
Dinesh Rao, MD, PhD
Elena Stark, MD, PhD
20 Years of Service
Sarah Dry, MD
25 Years of Service
Jonathan Said, MD
Graduating Trainees
Anatomic & Clincial Pathology Residency
Carlos Casiano, MD*
Jennifer Chia, MD, PhD
Katy Lawson, MD
Christine Lee, MD*
Trang Lollie, MD*
Michelle Phan-Tang, DO*
*Chief Resident
Cytopathology Fellowship
Maha Abdulla, MD
Yipeng Geng, MD, PhD
Dermatopathology Fellowship
Joan Leavens, MD
Alexander Nobori, MD
Klaus Lewin GI/Liver Fellowship
Ari Kassardjian, MD, PhD
Cherise Meyerson, MD
Hematopathology Fellowship
Robin Dietz Jr., MD
Neuropathology Fellowship
Zesheng Chen, MD, PhD
Surgical Pathology Fellowship
Bone and Soft Tissue
Farres Obeidin, MD
Genitourinary Pathology
Chunlai Zuo, MD
Genitourinary & Gynecologic Pathology
Jing Yang, MD, PhD
Women's Health Pathology
Sai Priyanka Gudiwada, MD
Olive View Medical Center
Mahdi Khoshchehreh, MD, MS
Ziming Tao, MD
Transfusion Medicine/CI Fellowship
Esteban Gnass, MD
Clinical Microbiology Fellowship
Evann Hilt, PhD
Travis Price, PhD
Immunogenetics Fellowship
Rebecca Sosa, PhD
Laboratory Genetics & Genomics Fellowship
Jaclyn B. Murry, PhD
Resident Housestaff Awards– Awarded by our Chief Residents
Conference Attendance
Jennifer Chia, MD, PhD
Precious Fortes, MD
Teresa Kim, MD
Katy Lawson, MD
Christine Lee, MD
Sofia Liou, MD
Trang Lollie, MD
Tara Narasimhalu, MD
Michelle Phan-Tang, DO
Rana Riahi, MD
Arash Roohani, MD
Jamar Uzzell, MD
Coverage King Award
Carlos Casiano, MD
Team Player Award
Teresa Kim, MD
Resident Teacher Award
Trang Lollie, MD
Social Chair Award
Tiffany Lin, MD
Office Parent Award
Trang Lollie, MD
Mission Impossible Award
Sarah Zhang, MD
The department is dedicated to fostering an environment that supports the mental and physical health of our Faculty, Trainees, and Staff. Our mission is to increase efficiency in the workplace, reduce stress, and provide resources to better manage an individual’s time and energy. We believe well individuals translate to a well team which in turn provides exemplary clinical care. We thank our department’s Wellness Officer, Dr. Stephanie Yang, for furthering our Wellness initiative, creating a detailed listing of available university resources, and being a champion for positive change. Please review and utilize our Wellness resources available on our website.
As we start anew, I look forward to our department focusing on Wellness practices in addition to our continued excellence and advancement in clinical care, education, and research.
June 2021
The Department of Pathology & Laboratory Medicine has placed great effort into our Quality Reboot over this past year. A highlight of these achievements include interdepartmental relationships, the Quality Culture and Education Committee, a focus on patient safety, and curriculum updates.
Interdepartmental relationships are the foundation of collaboration. I would like to spotlight some of the department’s collaborative efforts and projects:
- Dr. Shaun Yang, in collaboration with Dr. Annabelle de St. Maurice, Clinical Epidemiology and Infection Prevention, completed a quality improvement project to define a quantitative algorithm that helps with clinician decision making after inconclusive COVID-19 PCR results.
- Dr. Michelle Hickey and Melle Reider-Deimer, from the Department of Neurology, have initiated a quality improvement project to assess lab test utilization. The project aims to determine if clinician order practices can be protocolized to spare unnecessary test ordering.
- Dr. Rebecca Sosa and the Immunogenetics Laboratory have completed a quality improvement project to improve the turnaround time for virtual crossmatching for transplant patients. The aim of the project was to report virtual crossmatches within 1 hour to support OPTN requirements. Review and modification of communication and clinical protocols and technologist training has led to significantly increased efficiency, and 95% of VXM are reported within 1 hour, 4 months in a row.
- Dr. Alex Nobori completed a project that significantly reduced the time required to prepare cases for bone and soft tissue tumor board by developing and validating a Digital Tumor Board. The application reduced case preparation time from over 11 hours to just over 6 hours.
The Quality Culture and Education Committee (QCEP) is committed to improving the culture of quality throughout the Department of Pathology and Laboratory Medicine. By holding quality focused events such as Quality M and M and Quality Day, the committee seeks to elevate awareness, knowledge, and application of Quality Improvement methods for Faculty, Trainees, and Staff. The purpose of Quality M and M is to review adverse or near miss events, and consider the context, root cause analysis and corrective actions as a source of learning and improvement. This event aligns with UCLA Health’s goal of becoming a High Reliability “Zero Harm” organization. At the Quality M and M held in November 2020, two events originating from different areas of the laboratory, were discussed that directly impact patient safety. Dr. Nicole Valenzuela, and a group from the Immunogenetics Center, discussed the implications, root cause analysis and corrective actions of an event of transplant patient samples that were incorrectly accessioned. From Anatomic Pathology, Dr. Ryan Lau discussed the value of an IT project that improved the layout of interpretative comments in cytopathology reports to prevent misinterpretation.
In February 2021, the QCEP Committee held the annual Quality Day which included the 2021 Sarkaria Lecture by guest keynote lecturer Dr. Michael Astion, a clinical pathologist and Medical Director at the Department of Laboratories at Seattle Children’s Hospital and Clinical Professor of Laboratory Medicine and Pathology at the University of Washington. Dr. Astion’s lecture, entitled “Laboratory Stewardship: Achieving Alignment between Patients, Labs, and Payers” as well as the breakout sessions and workshops that followed, were attended by more than 100 people from our department via Zoom. Feedback from the day were extremely positive, highlighting the inclusivity of Faculty, Trainees and Staff, and the wide depth of topics covered in the schedule of events. The QCEP committee also seeks to highlight ongoing quality projects, and projects were presented by Dr. Alyssa Ziman (Division Chief, CP), Virgilio ‘Dindo’ Maglonzo (Flow Lab), Dr. Alex Nobori (Dermatopathology Fellow), Dr. Vishnu Samara (Clinical Pathology Fellow) and Dr. Rebecca Sosa (Immunogenetics Fellow).
Congratulations to Dr. Sophia Liou who is the recipient of a Good Catch Award for September 2020! Dr. Liou, a Surgical Pathology Resident in the department, identified a discrepancy between a patient’s clinical history and the order placed for her breast needle biopsy. The patient's clinical history and the surgical procedure noted that a right mass was to be biopsied. However, the breast needle biopsy was ordered as a left breast biopsy. Surgical pathology staff confirmed that the correct laterality should have been documented as RIGHT breast, and the Pathology records were updated to indicate the correct laterality. Dr. Liou’s critical examination of the documentation in this case was instrumental in preventing patient harm, and is an example of a commitment to the culture of safety at UCLA Health, and within the Department of Pathology.
During this past fiscal year, a new curriculum to support resident/trainee QI education was developed under the leadership of Dr. Yuna Kang. Using the existing structure of the resident lecture series, Dr. Kang invited members of the departments Faculty, Staff and Trainees to give lectures on quality topics that align with the Institute for Healthcare Improvement’s training modules for the Certificate in Quality Improvement. This educational series is also foundational to aid trainees in progress through the ACGME Resident Milestones for Patient Safety and Quality Improvement.
As this fiscal year comes to an end, I look forward to continued opportunities for collaboration, innovation, and excellence in research, education, and clinical care.
May 2021
As we welcome Spring, I would like to spotlight our clinical lab changes including our new anti-coagulation curriculum, total lab automation and robotics in the labs, our new specimen processing area in Ronald Reagan Hospital, and faculty updates.
Dr. Zhen Mei has created a new anti-coagulation curriculum to be implemented in the new fiscal year. The impetus to start a Coagulation Pathology rotation is 3-pronged. An opportunity was identified for improving the quality of residency education and experience based on subjective personal experience, past and current trainee feedback, and objective milestones from the ACGME. We are confident these objectives will fulfill the need for a standardized and consistent coagulation curriculum, improve resident perception of the level of coagulation training received during residency, and better prepare trainees in the assessment of coagulation issues and for their board examinations.
The Total Lab Automation (TLA) Project for the UCLA Health Clinical Laboratories is progressing on schedule. The BURL Laboratory is up and running on its new chemistry line, and both the Santa Monica Hospital Core Lab and the Ronald Reagan Hospital Core Lab are in the process of validation. Our new specialist group had a kickoff meeting where we brainstormed ideas for process improvement. In addition, the chemistry specialists from all three sites met to discuss validation/verification standardization. All of these initiatives and projects tie into the One Lab Philosophy as our Clinical Labs build the culture to see ourselves as one cohesive laboratory. Notably, the clinical lab has finished integrating the 200 Medical Plaza specimen processing area into the Ronald Reagan Core Lab specimen processing area. We want to thank everyone involved in that project and have already seen efficiency and patient care improvements. I also would like to thank Drs. Linda Baum and Omai Garner for their outstanding leadership of this significant project.
Additionally, I would like to congratulate Dr. Nam Ku on becoming our new Chief of Hematology and Dr. Linda Baum on her upcoming retirement.
We are excited for the new and innovative changes within the department and how they will positively impact our patients, trainees, the hospital, the university, and the community.
April 2021
The Department of Pathology & Laboratory Medicine is an integral part of the vibrant UCLA research enterprise and includes faculty members with a broad array of basic, translational, and clinical research interests.
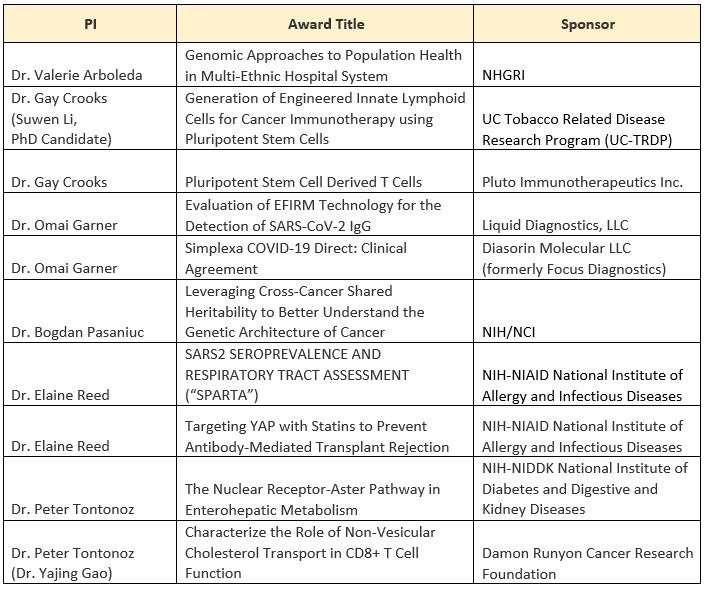
I am proud to profile our new research awards as of July 1st. We congratulate the faculty principal investigators on their grant awards and look forward to their innovative findings and results.
Departmental research has continued to thrive and grow over the past decade. Our faculty publish their findings in many of the top biomedical journals such as Cell, Immunity, Molecular Cell, Nature Immunology, and the Proceedings of the National Academy of Sciences. As a small representative snapshot, since March 2020, our faculty has produced over 250 published papers and abstracts. To date for FY2021, faculty researchers generated over $13 million in active extramural funding, including over $10 million from NIH. Learn more about a comprehensive listing of the department’s Faculty Publications.
Additionally, the department’s faculty is engaged in new collaborative work with other Departments and Schools at UCLA. Here are a few spotlighted collaborations:
- Dr. Valerie Arboleda is collaborating with Noah Zaitlen, in the Department of Neurology, to study Genomic Approaches to Population Health in Multi-Ethnic Hospital Systems. This project uses genomic information to reconstruct fine-scale population structure of different populations with EMR. In collaboration with Mt. Sinai School of Medicine and the University of Colorado, Dr. Arboleda and Dr. Gignoux are exploring how population-specific variants can influence clinical phenotypes. Additionally, in collaboration with the Dr. Butte and Dr. Krogstad at UCLA, the Valley Fever Institute seeks to identify some of the population-specific, genetic underpinnings underlying the immune dysregulation observed in disseminated coccidioidomycosis. This work is funded by University of California Office of the President.
- Dr. Kenneth Dorshkind has initiated a collaboration between the Dorshkind laboratory in the Department of Pathology and Laboratory Medicine and the laboratory of Dr. Sotirios Tetradis in the UCLA School of Dentistry. A goal of this collaboration is to determine how bone loss (osteoporosis) leads to age-related changes in the production of lymphoid and myeloid cells.
- Dr. Gregory Fishbein collaborates with UCLA pulmonary oncologists studying lung cancer preneoplasia, UCLA immunogeneticists studying heart and lung transplant rejection, and UCLA cardiologists studying medical devices.
- Dr. Oliver Hankinson initiated a new collaboration with Professor Jesus Araujo, UCLA Department of Medicine, on a grant they have submitted to the NIH to fund this research, which is titled “To test the hypothesis that activation of the Aryl Hydrocarbon Receptor will inhibit or promote atherosclerosis depending on the ratio of omega-3 to omega-6 polyunsaturated fatty acids in the diet”, and which is under review. He is also the contact PI on the renewal of the NIH T32 grant “Training in Molecular Toxicology”, which is currently under review. 14 faculty from 11 departments and 4 schools at UCLA are on the training grant faculty.
- Dr. Jeffrey Krane is collaborating with Dr. Maie St. John's group in the Department of Head and Neck Surgery to evaluate a novel imaging technique (DOCI) to better detect the presence of squamous cell carcinomas intraoperatively and guide diagnosis, treatment, and extent of surgery.
- Dr. Thomas Lawton is collaborating with: Dr. Greg Senofsky (Surgery) on a study comparing telomere length in benign breast biopsy patients who subsequently developed triple negative breast cancer and comparing to age-matched controls who had benign biopsies who did not go on to develop breast cancer; Dr. Jennifer Baker (Surgery) and two other institutions (UNC and UW) on a study looking at the natural history of in situ lobular neoplasia diagnosed at core needle biopsy; Dr. Helena Chang (Surgery) looking at CD44+/CD24high vs. low triple negative breast cancers and survival/response to neoadjuvant or adjuvant docetaxel-based chemotherapy; and Dr. Mary Sehl (Internal Medicine) on a study looking at adipose inflammation and DNA methylation age in women at high risk for breast cancer.
- Dr. Hane Lee has continued collaborative work within the Undiagnosed Diseases Network and California Center for Rare Diseases to identify molecular diagnosis for rare disease patients, including active research and developments around integrating transcriptome sequencing with whole genome sequencing data and increasing the efficiency of transcriptome sequencing. This collaborative work is not only for diagnosing rare disease patients, but also for founding the groundwork of bringing up whole genome sequencing and transcriptome sequencing as clinical tests in the Molecular Diagnostic Laboratories.
- Dr. Neda Moatamed is collaborating with several investigators at UCLA as a co-investigator, including: Triple-negative breast cancers (PI: Richard Pietras, MD); Abnormal cervical cytology in pediatric patients who have been vaccinated for HPV (PI: Anna-Barbara Moscicki, MD); and Platinum resistant ovarian cancer (PI: Sanaz Memarzadeh, MD, PhD).
- Dr. Bita Naini is collaborating on the PediCode consortium with Dr. Martin and Dr. Venick from Division of Pediatric Gastroenterology, Hepatology and Nutrition at UCLA as well as other academic centers. The Pediatric Congenital Diarrhea and Enteropathies Consortium (PediCODE) is a group of academic medical centers dedicated to research in rare genetic causes of early onset diarrheal disease and intestinal failure. UCLA is one of the four founding centers of this consortium and Dr. Naini is the director of pathology for UCLA site.
- Dr. Stanley Nelson collaborated with the Miceli Lab in MIMG, and within the Center for Duchenne Muscular Dystrophy, developed a novel muscle biopsy procedure coupled with a newly developed technique to purify individual nuclei to assess individual cell gene expression to identify novel cell types in muscle and changes in relation to lack of dystrophin in Duchenne and cellular responses from genomic medicines that restore dystrophin in skeletal muscle.
- Dr. Jian Yu Rao’s new collaborative works include: studying cancer cell mechanotypic biomarkers for cancer diagnosis and management; collaborating with Drs. James Gimzewski, Dino Di Carlo, and Amy Rowat from CNSI, a multicenter study for testing Computer-Aided System by Artificial Intelligence in the differential cell count on digital images of Bone Marrow Aspirates with pathologists from UT Southwestern; test the MUSE technology for rapid tissue analysis with pathologists from University of Rochester and Brigham and Women’s Hospital; Optimization of preanalytical variables affecting saliva ctDNA integrity and implications for use in clinical molecular testing with Dr. Liying Zhang and Dr. David Wong from UCLA Dental School; Optimization of preanalytical studies of HRD testing for ovarian cancer with Dr. Liying Zhang and Dr. Gottfried Konecny; and studying the associations of TMPRSS2 expression and COVID-19 disease with Dr. Liying Zhang, Dr. Huihui Ye, and Dr. Mathew Rettig.
- Dr. Elaine Reed is collaborating with Dr. Enrique Rozengurt, Department of Medicine and Director of CURE: Digestive Diseases Research Center and Dr. Robert Fairchild, Cleveland Clinic on a NIAID funded grant to study targeting YAP with statins to prevent antibody-mediated transplant rejection. The major goal of the research is to study the effect of donor specific HLA antibodies on the activation of the YAP/TAZ pathway in promoting proliferation and migration of ECs and to determine if drugs of the statin family inhibit YAP function in these cells. Dr. Reed, Matteo Pellegrini, and Michael Yeaman, collaborated on a study to unravel antibiotic resistance in MRSA “superbug” infections. The team identified 276 DNA sites in patients where methylation differed between those MRSA infections that were quickly resolved through the use vancomycin — one antibiotic that frequently is successful in combatting MRSA — and those infections that failed the antibiotic therapy. Pinpointing these epigenetic signatures at early diagnosis will enable physicians to predict which patients are likely to respond to a frontline antibiotic treatment for MRSA and which require different treatment strategies to clear the infection. This personalized approach also holds promise for improving outcomes for viral infections like COVID-19, HIV and influenza, as well as bacterial infections like tuberculosis, urinary-tract infections, and pneumonia. The findings were published March 1 in Proceedings of National Academy of Sciences. Additionally, a new study to determine whether preexisting immunity to SARS-CoV-2 can provide protection against repeat exposure has just opened at Harbor-UCLA, led by Dr. Elaine Reed. The Los Angeles SeroPrevalence And Respiratory Tract Assessment (LA SPARTA) study is funded by the NIH and supported by the UCLA CTSI. The study will enroll 100 front line providers who are health care workers, non-clinical Harbor UCLA employees, law enforcement, or paramedics and emergency medical service, representing the diverse racial and ethnic population of Los Angeles. Subjects will be tested by screening for symptoms of COVID-19, testing saliva for SARS-CoV-2, and monthly blood tests to evaluate the antibody response. This collaborative effort joins UCLA immunologic expertise of Dr. Reed and Infectious Diseases physician Dr. Joanna Schaenman, with the clinical and translational research expertise of Dr. Loren Miller and Dr. Michael Yeaman, collaborators from the Harbor-UCLA and the Lundquist Institute.
- Dr. Jonathan Said is engaging in a combined teaching and research conference with UCLA, UCSF, and Stanford for trainees and faculty in 2021.
- Dr. Shaun Yang is collaborating on multiple projects, including Candida auris genomic surveillance – working with the UCLA Department of Clinical Epidemiology and Infection Prevention (CEIP). Candida auris is an emerging multidrug resistant fungal pathogen causing outbreaks In the United States, and considered as one of five “urgent threats” to public health, prompting the need for active surveillance and appropriate infection prevention. Whole genome sequencing (WGS) based phylogenetic analyses can reveal the specific genotypes of C. auris and characterize its lineage and phylogenetic relationship with each other, therefore providing crucial information in helping with outbreak investigation and epidemiological studies. This study is an ongoing infection prevention and quality improvement project aiming to screen patients with C. auris colonization and infection and prevent its spread in the UCLA hospitals. He is also collaborating with the UCLA Department of Environment, Health and Safety (EHS) regarding COVID-19 campus surveillance by sewage testing. SARS-CoV-2 has been shown to be able to infect gastrointestinal tract and shed in stool for prolonged time after a patient is infected. Testing SARS-CoV-2 directly in the sewage has been shown to be capable of providing timely warning for potential outbreaks on college campus. They developed and validated a COVID-19 Stool PCR test that’s also working well for the sewage samples with high sensitivity, and have been using this test to help UCLA EHS to monitor the sewage samples, of which many tested positive during the COVID-19 winter surge in the LA area.
- Dr. Liying Zhang collaborated with Dr. Matthew Rettig, Medical Director of Prostate Cancer Program at Institute of Urologic Oncology, Dr. Andrew Goldstein in the departments of Molecular, Cell & Developmental Biology and Urology, as well as Dr. Huihui Ye and Dr. Jianyu Rao to study transcriptional inhibition of TMPRSS2 and received a COVID-19 research award from the Broad Stem Cell Center/School of Medicine; with Dr. David Wong in School of Dentistry to develop new methods for detecting COVID-19 infection and received NIH grant; with Dr. Edward Garon in Department of Medicine to study preanalytical variables affecting saliva ctDNA integrity and implications in clinical testing and submitted NIH U01 grant; with Dr. Timothy Donahue in Department of Surgery to study ctDNA in pancreatic cancer; and with Dr. Gottfried E. Konecny to develop assays for HRD detection in ovarian cancer.
- Dr. Alyssa Ziman has collaborated on: COVID-19 Convalescent Plasma (CCP) – Developed collaborative research program with Division of Infectious Disease and Clinical Research enterprise to recruit and screen individuals who had recovered from COVID-19 for participation in immunology research and as convalescent plasma donors. Also developed comprehensive donor recruitment and screening processes to collect and manufacture CCP for transfusion under an EUA for hospitalized patients and for various clinical research protocols in the outpatient and emergency department settings; Research on Novel Blood Components.
- Division of Neuropathology – The Division of Neuropathology continues collaboration with multiple clinical and research colleagues in neurosurgery, neurology and the Mary S. Easton Center for Alzheimer disease research.
- Division of Transfusion Medicine – The Division of Transfusion Medicine is collaborating with our clinical colleagues on several studies to evaluate novel blood products (Whole Blood for Cardiac Surgery, Pediatric Cardiac Surgery and Pediatric Intensivists; Pathogen Reduced RBCs, Adult Cardiac Surgery; Cold-Stored Platelets, Anesthesia); and the Bruin Blood Initiative: Providing mentorship for the Bruin Blood Initiative, an undergraduate UCLA club focused on blood donor education and recruitment. The Transfusion Medicine faculty is proving mentorship to club members on a research project aimed at analyzing blood donor demographics and donation trends at a college donor center.
The above publications, grants and collaborations underscore that UCLA is a highly interactive and collaborative environment in which interdisciplinary research flourishes. I am grateful that, despite the challenges of the last year, our faculty and students have continued to conduct important and meaningful basic, translational and clinical research and I look forward to learning about their future discoveries.
March 2021
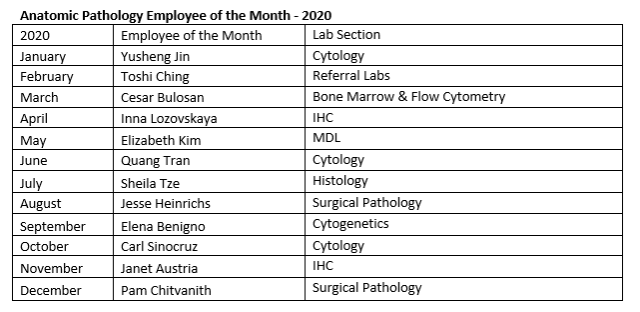
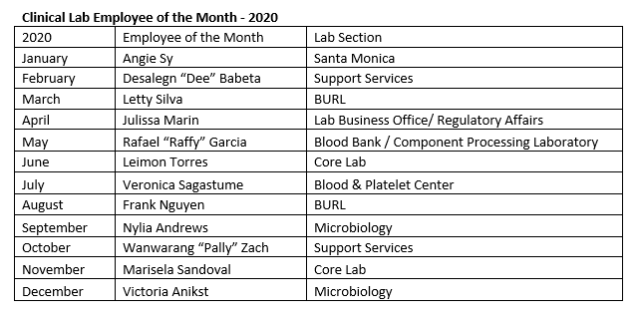
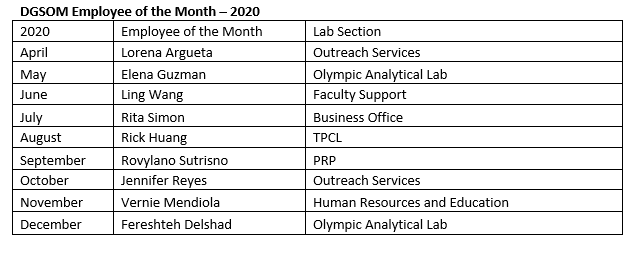
Each day we strive to uphold the UCLA mission to heal humankind by delivering leading-edge research, education, patient care, and community engagement. In light of our departmental achievements toward these goals, I would like to spotlight our monthly Staff Recognition Program. We thank these amazing individuals for their hard work, dedication, and excellence.
Our department takes immense pride in our continued outreach to better serve the community. These contributions include the Light the Night, I Heart Walk, and so much more. Please see the detailed listing below.
Blood & Platelet Center and Transfusion Service
- COVID-19 Pandemic
- COVID-19 Convalescent Plasma (CCP):
- Collected CCP from 250+ unique donors in 400+ visits
- Collected 1,200+ CCP units
- Transfused approx. 20 patients as part of the Johns Hopkins CCP study
- Transfused 240+ UCLA patients as part of the Mayo study and then under the Extended Use Authorization (EUA)
- Shipped 500+ CCP to other hospitals as part of the Mayo study
- COVID-19 Convalescent Plasma (CCP):
- Transfusion Service
- Milestones:
- 1st UC to have a permanent Transfusion Safety Officer position (Floricel Guillermo)
- RRUCLA achieved Magnet Designation with the help of our Transfusion Safety Officer
- Milestones:
- Community Engagement
- Lab Tours for the DGSOM Medical Students throughout the year
- Bethany Porter presented CLS career information at multiple events for UCLA Health and UCLA Alumni
- Ed Griffin presented a webinar for AABB on Leading Through Change
- Floricel Guillermo presented at Marymount High School in promotion of blood donation
- Floricel Guillermo led a blood drive during nurses week with a total of 72 nurses who donated
Brentwood (Microbiology/Serology/Virology)
- Milestones
- Performed over 175,000 COVID PCR tests by the end of the year (next highest test volume is ~70,000 tests/year)
- Community Engagement
- Provided COVID-19 testing for people in the community experiencing homelessness
- Were featured by the World Series winning Dodgers saying, “It’s Time for Dodger Baseball” before a game
- Several LA Times articles have featured our laboratory
- Members of our lab appeared in an ASCP Townhall video discussing the Coronavirus pandemic
Community Event Participation
American Heart Association Virtual Walk
- The event aims to fund lifesaving science and promote the Health For Good movement.
- Lab Team Captain Nathan Okawa raised $9336
I Heart Walking
- The event promotes heart health through prevention education and healthy practices.
- 14th annual event
- Held on February 12, 2020
Light the Night Event
- The Leukemia & Lymphoma Society's Light The Night Walk funds treatments that are saving the lives of patients today. LLS is making cures happen by providing patient support services, advocating for lifesaving treatments, and pioneering the most promising cancer research anywhere.
- Organized by Tom Callahan, Brian Ahrens, Deanna Fang, Cristina Ghiani, Ronald Gonzalez, Yulia Kucherova, Nathan Okawa, and Nikki Salami
Core Lab
- Community Engagement
- Lab Tours for the DGSOM Medical Students throughout the year
Regulatory Affairs
- 7 CLS students graduation, 8 CLS students onboarded
- 1 CGMBS student graduated
UIC
- Clinical
- Provided Histocompatibility and Immunogenetic testing for 1,236 solid organ transplants for the 5 transplant centers we serve (UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange) and 850 deceased donor workups for One Legacy, the Organ Procurement Operation for Los Angeles
- Provided Immunogenetics and Histocompatibility testing for >90 kidney paired donations at UCLA
- Added value and standardization to living and deceased donation workflows by providing written reports of virtual crossmatches to transplant centers
- Increased clinical footprint
- Providing deceased non-renal donor crossmatch services for 2 additional outside transplant centers
- Developed strategy to address UNOS Policy change eliminating donor areas and affecting deceased donor transplants. UIC will manage and perform deceased donor crossmatch services for 8 Los Angeles transplant centers.
- Educational
- Provided 3 educational lecture series via Zoom for physicians, fellows, residents, and coordinators at UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange, One Legacy, and Kaiser
- Created a library of recorded lectures to be able to provide training on demand
- Research
- Work with faculty and fellows for publications and obtaining grants
- 4 new NIH Grants and 31 publications
- Recruitment
- Yuxin Yin, Project Scientist, Research and Development for assay development and translating research findings to diagnostic testing
- IT Integration
- Designed, validated and put into production order/reporting interface for 2 transplant programs
- Reference Program
- UIC serves as CAP proficiency test provider since 2003
- UIC received 100% Supplier Report card from CAP in 2020
Despite the changes we have endured due to COVID-19, hope and perseverance shine as brightly as our hard work and determination to serve the university, hospital, community, and beyond. I am proud of our accomplishments this past year and look forward to all we will achieve in the academic, clinical, and research arenas.
February 2021
In the spirit of the new year, I would like to spotlight our departmental education programs and contributions. The David Geffen School of Medicine and the Department of Pathology & Laboratory Medicine strive to provide opportunities for world-class education, training, and professional development. We foster and cultivate a rich learning environment that prepares each individual for the next steps on their chosen career path. The associated lists below provide a snapshot of our many programs and affiliations. We are proud of our accomplishments in the educational arena and continue to revolutionize our curriculum, programs, and clinical work.
Additionally, I would like to extend my congratulations to Dr. Dipti Sajed on her new appointment as Anatomic Pathology Associate Program Director!
This position will have a primary responsibility of overseeing the educational content of the AP program, including the resident curriculum, rotation goals/expectations, and conferences. The AP APD will function independently, but will also work closely with the Program Director to assist in other aspects of the program including recruitment, clinical competencies, and real-time issues raised by trainees, faculty, or staff. Recent improvements to the educational program since the her appointment include: a new PGY1 frozen section rotation to ensure adequate training for on-call duties, a quality and content update of the official AP conference curriculum, and an increase in efficiency of clinical competency committee meetings.
As we move forward in 2021, I encourage you to participate in opportunities to enhance your learning experience and professional development. Education, collaboration, and continued learning are the foundation of the field of medicine. May the new year bestow discovery, innovation, and exemplary clinical care.
Non-MD/DO/PhD Clinical Training Programs
MD/DO ACGME Clinical Training Programs
MD/DO/PhD Non-ACGME Clinical Training Programs
December 2020
As we approach the new year, I would like to highlight some of our department's achievements in 2020.
The Department of Pathology and Laboratory Medicine's One Lab Philosophy encompasses the innovation, dedication, and continuity within our laboratory structure. Our strategy within UCLA Health is we are one lab with many sites, including Santa Monica, Brentwood, BURL, CHS, and Ronald Reagan. We share methodology, operating procedures, project prioritization, and informatics; our new Vice Chair for Clinical Lab Strategy, Dr. Omai Garner, is working very closely with faculty and senior staff to ensure that internally and externally, to our vendors and clients, we all work as one lab.
This one lab approach will enhance our ability to provide the best care for our patients, while acting as good stewards of the resources provided to us. We appreciate the expertise of our managers, supervisors and specialists at all of our sites, and will continue to maximize the ability of staff to work across our sites to share experience and best practices. The One Lab Committee's next immediate focus is to spearhead the rebranded quarterly Pathology Newsletter and host additional faculty discussions and forums.
In the spirit of the holiday season, I would like to express my immense gratitude for the incredible support, effort, energy, and creativity our department has shown since the emergence of COVID-19. Despite unprecedented changes to all facets of our daily lives, our team has persisted in doing everything they can to help our patients, clinicians, and each other. The department has ensured that we have continued to deliver outstanding clinical care, found creative ways to provide critical education remotely and in person to medical students, residents, fellows, and technicians, and have persevered to make research discoveries, submit grants, and publish papers.
I look forward to our continued excellence and advancement in clinical care, education, and research in the new year.