Skin Changes of the Breast
By: Irvin Calderon M.D. and Melissa Joines M.D.
Skin changes of the breast are a common reason for breast consultation and imaging evaluation. The most common manifestations of skin changes include scaling, dimpling, swelling, nodules, rashes, erythema, and symptoms of itching, with most etiologies being of a benign nature. A few common causes of skin changes include infection, inflammatory breast disease, and malignancy.
Infection
One of the most common etiologies of benign skin changes of the breast is due to infection, which is often categorized based on the patient’s lactational status because of inherently increased risk for infection. Infection solely confined to the breast skin is considered breast cellulitis. The most implicated pathogens are group A streptococcus and methicillin-sensitive Staphylococcus aureus, which generally respond well to antibiotics. Fungal pathogens may be responsible for skin infection in cases of unresolved cellulitis or in immunocompromised patients. An unresolved breast infection can progress to infectious mastitis which can then develop a breast abscess or mammary fistulae, with a complication rate up to 11% and 2%, respectively.
Infection involving breast parenchyma is considered infectious mastitis. Infections during lactation or in the 6-week post-lactation period, are considered puerperal infections. Infectious mastitis is considered the most common benign breast pathology in pregnancy and puerperium, carrying the highest incidence during the first few weeks postpartum.
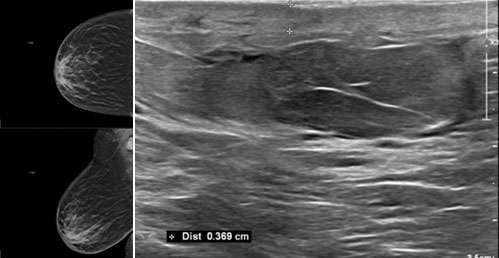
Imaging is indicated in cases of unresolved or persistent infection of the breast to evaluate for an abscess or other etiologies, and for therapeutic purposes such as image-guided aspiration. Ultrasound is usually the first indicated imaging modality that is tailored to the signs and symptoms, with findings that include dilated ducts, heterogeneous tissue related to diffuse inflammation and edema, and organizing fluid collections.
Currently, there are no official recommendations for the use of mammography for evaluation of breast infection unless there is suspicion of an underlying malignancy. Mammography should occur after the resolution of the acute phase of infection to allow patients to undergo compression images, resulting in the optimization of these images and leading to a better diagnostic yield.
Mammographic findings in patients with mastitis and in those with an abscess include asymmetric density, skin thickening, and a mass if an abscess is present. The presence of suspicious appearing microcalcifications is unusual for breast infection and should prompt further evaluation and biopsy to exclude an underlying malignancy. Similarly, unresolved findings after treatment may warrant histopathologic evaluation.
MRI has minimal utility in differentiating infection from malignancy given considerable overlap of findings.
Non-infectious/inflammatory changes
Non-infectious mastitis is often a result of inflammatory conditions including duct ectasia, granulomatous mastitis, a foreign body reaction, or dermatologic conditions that either uniquely or incidentally involve the breast.
Duct ectasia (also called peri-ductal mastitis or plasma cell mastitis) is an idiopathic disease process affecting the large duct system, and is characterized by elongated, convoluted, and weakened duct walls, which may present with associated nipple discharge or a palpable mass.
Granulomatous mastitis is an idiopathic chronic inflammatory breast disease commonly occurring in women of child-bearing age. Causes are debated but thought to be related to autoimmunity versus chronic infection. It is considered a clinical mimic of inflammatory breast cancer and periductal mastitis, often necessitating histopathologic evaluation, and is characterized by non-caseating granulomas and microabscesses.
A foreign body reaction of the breast can be induced by objects such as nipple piercing, breast implant, or silicone.
Lastly, dermatitis of the breast may be caused by several etiologies, including atopic dermatitis and radiation-induced dermatitis.
Atopic dermatitis (eczema) affects the breast and nipple in approximately less than 20% of patients with a history of eczema. It is the cause of approximately half of breast dermatitis cases that occur during breastfeeding in patients with a medical history of eczema. The breast skin findings are identical to atopic dermatitis that occurs elsewhere in the body, mostly occurring bilaterally, and often with concurrent systemic involvement. Eczema of the nipple frequently flares during breastfeeding, with a higher associated risk for superimposed infection due to excoriation or cracking of the nipple from nursing.
Dermatitis occurs in nearly all patients who undergo radiotherapy for breast cancer and occurs within 3 months of radiation exposure. It ranges in severity from mild erythema to full-thickness skin necrosis. The disease process peaks for up to 2 weeks and may take up to 4 weeks to resolve after treatment.
Often, the diagnosis of inflammatory causes of breast skin changes can be made on clinical grounds. When imaging is performed, mammographic and ultrasound findings are nonspecific and similar to the findings listed above for infection of the breast (Figure 1). The role of imaging in these cases is to evaluate for or exclude malignancy.
Malignancy
Given the significant overlap of presentation between mastitis and inflammatory breast cancer, if the findings persist after appropriate treatment of presumed infection or other diagnosis, the work-up of malignancy should be pursued. A few notable examples of breast malignancy with associated skin changes include inflammatory breast cancer, Paget’s disease of the breast, and metastatic versus non-metastatic skin changes secondary to primary breast cancer.
Inflammatory breast cancer is an aggressive form of breast cancer that accounts for approximately 5% of breast malignancies. There are no definitive molecular or pathological diagnostic criteria, making the diagnosis reliant on clinical symptoms, which are characterized by rapid onset of signs of breast skin changes.
Although erythema and swelling can be seen in mastitis and inflammatory breast cancer, more advanced skin finding, such as the “peau d’orange” appearance, is more concerning and specific to inflammatory breast cancer appearance. Additional work-up includes biopsy and imaging to evaluate disease extent.
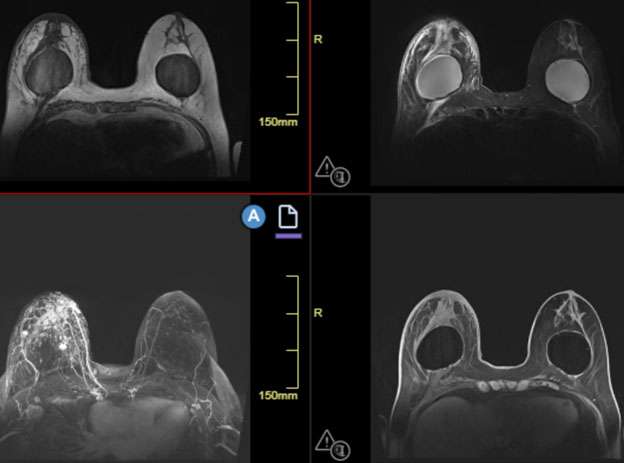
Imaging entails a diagnostic mammogram of the affected breast, screening mammogram of the contralateral breast, and corresponding ultrasounds of the breasts and axilla, with tailoring of the examination if a palpable or focal abnormality is present.
The mammographic findings of inflammatory breast cancer include nonspecific, but suspicious, findings of a mass, calcification, distortion, and skin thickening.
The ultrasound findings of inflammatory breast cancer include skin thickening, presence of interstitial fluid, and distortion. Furthermore, ultrasound is particularly useful for the evaluation of regional nodal disease.
Challenges in imaging inflammatory breast cancer are related to the degree of edema, causing patient discomfort. This may prevent optimal images from being acquired, such as a mammogram with compression views. Additionally, a primary breast lesion may be obscured because of the presence of significant skin and parenchymal thickening.
When MRI is performed, findings may include a heterogeneously enhancing mass and skin thickening. MRI is the most accurate imaging technique in detecting primary breast parenchymal lesions in cases of inflammatory breast cancer and may assist in delineation of disease extent (Figure 2).
FDG PET/CT has added utility in assessing for regional lymph node disease or distant metastatic disease, and to assess for treatment response.
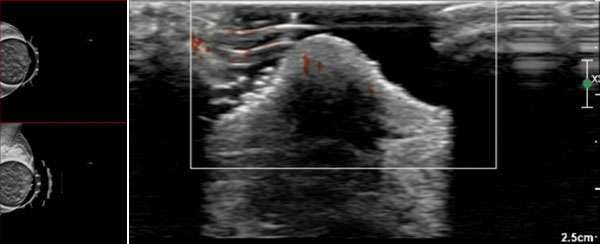
Paget’s disease is a malignant disease process with corresponding skin changes and imaging features that account for approximately 3% of breast malignancies. The disease commonly occurs in postmenopausal women. Almost 80-90% of cases are associated with underlying malignancy, usually in the form of ductal carcinoma in situ or invasive breast cancer.
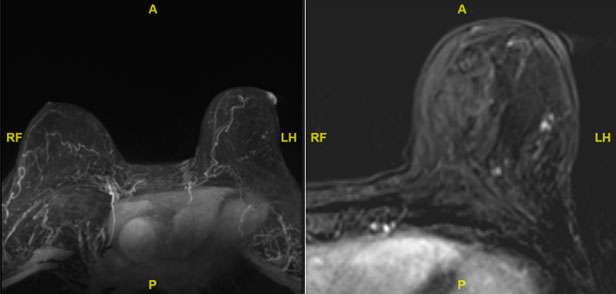
The most associated skin changes in Paget’s disease include a lump, nipple pain, nipple discharge, and more specifically scaly or plaque-like skin changes at the nipple-areola complex. Typically, after the diagnosis of Paget’s disease is made via skin biopsy, breast imaging is utilized for the diagnosis of an underlying primary breast cancer, similar to the imaging work-up of inflammatory breast cancer.
The mammographic findings of Paget’s disease include skin thickening in the nipple areolar complex region, nipple retraction, underlying suspicious calcifications, or a discrete mass. The ultrasound findings include nonspecific heterogeneity of the breast parenchyma, a mass, dilated ducts, and skin thickening or hypervascularity in the nipple areolar complex (Figure 3). Breast MRI may assist in further evaluation in the setting of negative mammogram and ultrasound findings (Figure 4).
Lastly, while inflammatory breast cancer and Paget’s disease of the breast are the prototypical malignant breast entities with well-described skin changes, other types of skin changes can develop from breast cancer, either from direct or contiguous spread in the setting of skin metastasis versus non-inflammatory involvement.
Breast cancer is the most common source of skin metastasis. In metastatic disease, breast skin lesions that raise the alarm for metastatic involvement include nonhealing ulcers, persistent indurated erythema, and unexplained skin nodules. Additional rare manifestations include a varicella-zoster type presentation as a vesicular rash, and diffuse sclerodermoid indurations with invasion of the chest wall that create an appearance called “carcinoma en cuirasse,” which resembles a medieval breastplate.
Non-inflammatory skin changes from breast cancer include skin tethering due to infiltration of Cooper’s ligaments. This process creates dimpling or puckering of the overlying skin. When tethering involves the nipple, it can lead to nipple retraction. This should be differentiated from benign nipple inversion, which may be seen in the setting of post-surgical changes and fibrocystic changes. If further work-up is necessary, combined mammogram and ultrasound can evaluate structural changes due to an underlying malignancy. Given its high sensitivity, MRI can be used in cases of both negative mammography and negative ultrasound findings. MRI findings of breast cancer skin changes include thickening and irregular enhancement of the nipple-areolar complex, detection of an underlying mass, or suspicious enhancement.
References
- Boakes E, Woods A, Johnson N, Kadoglou N. Breast Infection: A Review of Diagnosis and Management Practices. Eur J Breast Health. 2018 Jul 1;14(3):136-143. DOI: 10.5152/ejbh.2018.3871. PMID: 30123878; PMCID: PMC6092150.
- Brown BD, Hood Watson KL. Cellulitis. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 31747177.
- Chippa V, Barazi H. Inflammatory Breast Cancer. 2023 Apr 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 33231994.
- Crowe DJ, Helvie MA, Wilson TE. Breast infection. Mammographic and Sonographic Findings with Clinical Correlation. Invest Radiol. 1995 Oct;30(10):582-7. PMID: 8557497.
- Culver AL, Metter DM, Pippen JE Jr. Carcinoma en cuirasse. Proc (Bayl Univ Med Cent). 2019 Mar 26;32(2):263-265. DOI: 10.1080/08998280.2018.1564966. PMID: 31191149; PMCID: PMC6541069.
- Hamwi MW, Winters R. Mammary Duct Ectasia. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32491597.
- Hudson-Phillips S, Cox K, Patel P, Al Sarakbi W. Paget's Disease of the Breast: Diagnosis and Management. Br J Hosp Med (Lond). 2023 Jan 2;84(1):1-8. DOI: 10.12968/hmed.2022.0439. Epub 2023 Jan 24. PMID: 36708338.
- Lim HS, Jeong SJ, Lee JS, Park MH, Kim JW, Shin SS, Park JG, Kang HK. Paget Disease of the Breast: Mammographic, US, and MR Imaging Findings with Pathologic Correlation. Radiographics. 2011 Nov-Dec;31(7):1973-87. DOI: 10.1148/rg.317115070. PMID: 22084182.
- Lookingbill DP, Spangler N, Sexton FM. Skin Involvement as the Presenting Sign of Internal Carcinoma. A Retrospective Study of 7316 Cancer Patients. J Am Acad Dermatol. 1990 Jan;22(1):19-26. DOI: 10.1016/0190-9622(90)70002-y. PMID: 2298962.
- Mahoney MC, Ingram AD. Breast Emergencies: Types, Imaging Features, and Management. AJR Am J Roentgenol. 2014 Apr;202(4):W390-9. DOI: 10.2214/AJR.13.11758. PMID: 24660738.
- Mamouch F, Berrada N, Aoullay Z, El Khanoussi B, Errihani H. Inflammatory Breast Cancer: A Literature Review. World J Oncol. 2018 Nov;9(5-6):129-135. DOI: 10.14740/wjon1161. Epub 2018 Nov 23. PMID: 30524636; PMCID: PMC6279456.
- Nagaraja Rao D, Winters R. Inverted Nipple. 2023 Jul 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 33085337.
- Pickett H. Shave and Punch Biopsy for Skin Lesions. Am Fam Physician. 2011 Nov 1;84(9):995-1002. PMID: 22046939.
- Putra HP, Djawad K, Nurdin AR. Cutaneous Lesions as the First Manifestation of Breast Cancer: A Rare Case. Pan Afr Med J. 2020 Dec 29;37:383. DOI: 10.11604/pamj.2020.37.383.27380. PMID: 33796196; PMCID: PMC7992436.
- Salzman B, Fleegle S, Tully AS. Common Breast Problems. Am Fam Physician. 2012 Aug 15;86(4):343-9. PMID: 22963023.
- Sripathi S, Ayachit A, Kadavigere R, Kumar S, Eleti A, Sraj A. Spectrum of Imaging Findings in Paget's Disease of the Breast-A Pictorial Review. Insights Imaging. 2015 Aug;6(4):419-29. DOI: 10.1007/s13244-015-0415-z. Epub 2015 Jul 5. PMID: 26142549; PMCID: PMC4519816.
- Tan H, Li R, Peng W, Liu H, Gu Y, Shen X. Radiological and Clinical Features of Adult Non-puerperal Mastitis. Br J Radiol. 2013 Apr;86(1024):20120657. DOI: 10.1259/bjr.20120657. Epub 2013 Feb 7. PMID: 23392197; PMCID: PMC3635790.
- Waldman RA, Finch J, Grant-Kels JM, Whitaker-Worth D. Skin Diseases of the Breast and Nipple: Inflammatory and Infectious Diseases. J Am Acad Dermatol. 2019 Jun;80(6):1483-1494. DOI: 10.1016/j.jaad.2018.08.067. Epub 2018 Nov 16. PMID: 30452953.
- Yasir M, Khan M, Lotfollahzadeh S. Mammary Paget Disease. 2023 Jun 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 33085375.
- Yin Y, Liu X, Meng Q, Han X, Zhang H, Lv Y. Idiopathic Granulomatous Mastitis: Etiology, Clinical Manifestation, Diagnosis and Treatment. J Invest Surg. 2022 Mar;35(3):709-720. DOI: 10.1080/08941939.2021.1894516. Epub 2021 Mar 10. PMID: 33691563.