Intestinal Rehab & Care
Find your care
At UCLA Health, you’ll have an experienced team of transplant specialists who deliver coordinated, expert care. Call 310-825-8138 to connect with us.
At UCLA, we provide expert nutritional care and intestinal rehabilitation to assess and improve small bowel function for patients with intestinal failure and short bowel syndrome (also known as short gut syndrome).
Our comprehensive program includes pediatric intestinal rehabilitation.
What Is Intestinal Rehabilitation?

Intestinal rehabilitation seeks to improve the function of the existing small bowel in patients with intestinal failure.
Our expert teams work with patients who have a variety of conditions that cause intestinal failure, including short bowel syndrome (short gut syndrome) and intestinal injury.
Many of these patients rely upon TPN (total parenteral nutrition). Unfortunately, TPN can cause serious complications after long-term use, including:
- Liver disease
- Central venous catheter (CVC) infections
- Loss of CVC sites
- Major fluid and electrolyte imbalances
Intestinal rehabilitation aims to help you avoid TPN's complications and regain a normal life - ideally, allowing you to begin or resume eating food.
Options for Intestinal Failure at UCLA
UCLA provides the complete range of care for patients who experience intestinal failure.
Our intestinal care program includes:
- Nutritional management and TPN (total parenteral nutrition) management
- Autologous reconstructive surgical options (surgery of existing intestinal structures)
- Medical therapies
- Transplantation, including pediatric intestinal transplant, adult intestinal transplant, liver transplant and other organ transplants
What Is Short Bowel Syndrome?
Short bowel syndrome refers to a condition where the intestinal tract no longer absorbs nutrients. This condition results in malabsorption, diarrhea and malnutrition. It is also known as short gut syndrome.
Causes of short bowel syndrome include:
- Being born with malformations of the small intestine (small bowel) that cause short bowel syndrome
- Illness (such as Crohn's disease)
- Injury or surgery that involves removal of part of the small intestine
- Problems that prevent the gut from correctly digesting, absorbing and moving food through the intestinal tract (functional disorders)
- Having a combination of any of the above
In some cases, short bowel syndrome is temporary. For these patients, the remaining intestine adapts, allowing them to once again digest and absorb all nutrients through the gastrointestinal tract. This process involves:
- Adaptation begins soon after the onset of short bowel syndrome.
- Adaptation may not be complete for several years.
- Whether your small bowel can adapt depends on your health, age, length of remaining intestine, presence or length of colon, and presence or absence of disease in the remaining intestine.
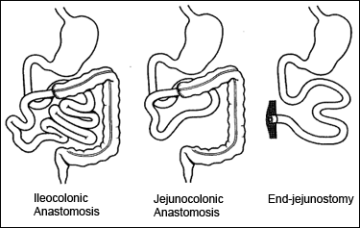
From Feldman: Sleisenger & Fordtran's Gastroentestinal and Liver Disease;
7th Edition; Figure 92-1, page 1808; 2002, Elsiever
Your physician will advise you on the potential of your intestine to adapt.
Unfortunately, some patients do not adapt from short bowel syndrome. Such patients require total parenteral nutrition (TPN) for the rest of their lives. This condition is called intestinal failure.
What Is Total Parenteral Nutrition (TPN)?
Total parenteral nutrition (TPN) is a liquid form of calories and nutrients given intravenously.
TPN is a life-saving option for patients who develop short bowel syndrome and intestinal failure. After years of formulation and experience starting in the 1960s, TPN is a safe and effective way to provide life-sustaining nutrients to patients who cannot absorb these calories and nutrients via the gastrointestinal tract.
Risks of TPN
Up to 80 percent of patients can use TPN with few or no complications. However, TPN does carry some risks. You and your physician will discuss whether TPN is the best option for you.
When complications increase so that TPN is no longer an option, a patient may be eligible for adult intestinal transplant or pediatric intestinal transplant. These complications may include:
- Liver disease: Some patients develop liver disease, which can result in end-stage liver disease or cirrhosis. This condition requires transplantation. UCLA is recognized as a world leader in both adult liver transplant and pediatric liver transplant. Our liver and intestinal transplant teams work together very closely to support these patients.
- Central venous catheter (CVC) infections: Multiple, recurrent infections can result in having to remove the CVC. These infections can be severe or even life-threatening.
- Loss of CVC sites: Adults generally have 6-8 standard venous access sites, while children have 4-6. When a patient's vein develops clotting so that a catheter cannot be replaced in that vein, it is considered permanently lost. Losing more than half of your access sites can affect your long-term ability to receive TPN.
- Major fluid and electrolyte imbalances: Patients with these imbalances can become dehydrated or develop renal failure.
Many patients succeed well with TPN. Our team will work with you to determine the best treatment plan for your condition.