While there have historically been few options to treat persistent atrial fibrillation (A-fib), a recent partnership between electrophysiologists and cardiac surgeons at UCLA Health is putting patients’ hearts back in sync.
A healthy heart beats steadily, with each contraction pushing blood from its upper chambers (the atria) to its lower chambers (the ventricles), which then pump blood to the rest of the body. But in a person with A-fib, a common heart arrhythmia, electrical signals go awry — the atria contract rapidly out of sync with their southern counterparts.
At first, this irregular heart rhythm occurs as brief episodes, and may cause minimal symptoms. However, A-fib events usually increase over time, sometimes causing patients to experience fatigue, shortness of breath, and palpitations. In rare cases, A-fib may cause heart failure or contribute to the risk of dementia. Left untreated, A-fib can significantly raise a person’s risk of having a stroke in their lifetime.
“A-fib is easiest to treat soon after it starts. But patients might not be bothered by short episodes of irregular rhythm and might not seek treatment,” says Eric Buch, MD, a cardiac electrophysiologist at the UCLA Cardiac Arrhythmia Center. “Over months or years, the A-fib becomes persistent, and this causes changes in the atria that make it harder to treat.”
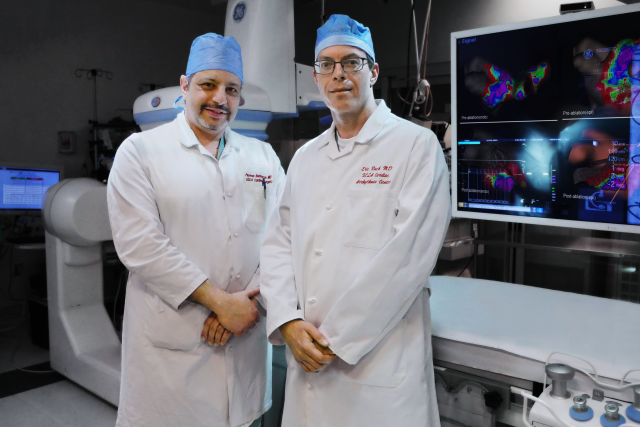
The new, two-stage, minimally invasive procedure that Dr. Buch can now offer his patients is called hybrid convergent ablation. By treating both the inside and the outside of the heart, hybrid ablation blocks abnormal electrical signals to provide a more effective treatment for long-standing, persistent A-fib.
Improving on old methods
In the recent past, A-fib was typically treated via two methods: antiarrhythmic drugs, which are less effective and have potential side effects, and an ablation procedure, in which catheters are guided through blood vessels into the heart to freeze or heat the tissue that causes A-fib.
Catheter ablation works well in the early stages of A-fib, but is less effective when the rhythm is persistent, says Dr. Buch. When delivering energy to the inside of the heart, electrophysiologists must carefully avoid causing collateral damage to the structures near the heart, like nerves or the esophagus. For a patient with persistent A-fib for more than a year, the success rate of the catheter ablation procedure is less than 50%.
However, even for these long-standing A-fib patients, a surgery called the maze procedure can have better, more long-lasting results. During this procedure, a cardiac surgeon creates a “maze” of scar tissue in the heart’s atria using a tool that delivers hot or cold energy. This interferes with the electrical heart signals that cause A-fib. But while the maze procedure is very effective, the surgery is invasive, and the recovery is long.
By combining a minimally invasive version of this surgery with a catheter ablation, cardiac surgeons and electrophysiologists can team up to treat both the outside and the inside of the heart. In 2020, the results of the CONVERGE clinical trial showcased the effectiveness of the hybrid method compared to catheter ablation alone.
“This hybrid option leverages the best of both technologies,” says Peyman Benharash, MD, a cardiac surgeon at UCLA Health.
How it works
First, Dr. Benharash performs surgery on the outside of the heart. Rather than performing a full open-heart surgery, he makes small incisions on the chest, inserts a thoracoscope, and uses a camera to guide the minimally invasive ablation on the outside of the atrial wall. Recovery time in the hospital, on average, is two or three days.
Around eight weeks after surgery, the patient returns to UCLA Health. That’s when Dr. Buch or another electrophysiologist completes the procedure with a catheter ablation. By carefully mapping the work already done by Dr. Benharash, energy can be applied only where it’s needed to complete the ablation. This second part, also called endocardial ablation, is usually done as an outpatient procedure.
So far, UCLA doctors have performed the hybrid procedure more than 60 times. They estimate that over 80% of their patients have remained in normal rhythm post-surgery. The procedure also has an added benefit of lowering stroke risk by closing the part of the atrium where blood clots can form.
What both clinicians want referring cardiologists, patients, and other physicians to know is that this can be a good treatment option for many patients with persistent A-fib.
”It may not be widely understood that hybrid ablation is very different from traditional maze surgery for A-fib, and it’s very different from catheter ablation,” Dr. Buch says. “It’s much less invasive than the maze procedure, and more effective than catheter ablation alone.”
For Dr. Benharash, that’s a real game-changer.
“This opens up treatment to many, many patients who never before had options to treat their persistent A-fib,” he says. “And I think that is pretty remarkable.”
Lauren Ingeno is the author of this article.