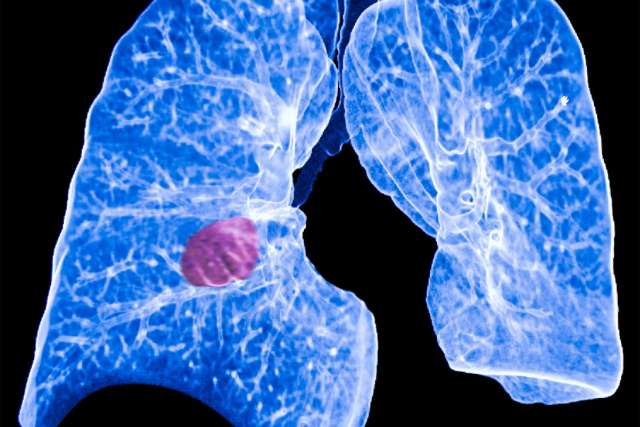
Most people at greatest risk of lung cancer are overlooking a non-invasive screening that can detect cases early, when treatment can best save lives.
November marks Lung Cancer Awareness Month and UCLA Health lung cancer experts are working to spread the word about the importance of low-dose computed tomography (LDCT) of the chest. The annual scan is recommended for people with a long-term history of smoking, as well as other criteria, including age.
The screening is designed to find asymptomatic cancers when they are most treatable with surgery or radiation. It also allows doctors to monitor any suspicious findings over time.
Denise Aberle, MD, a distinguished professor of radiology at the David Geffen School of Medicine at UCLA, led the National Lung Screening Trial that established the superiority of low-dose CT scans over standard chest X-rays. Participants who had the CT scan had a 20% lower chance of dying from lung cancer, according to the findings published in 2011.
“There are a number of breakthroughs that have happened with respect to lung cancer, which was historically an almost uniformly fatal disease because it was always diagnosed late,” said Dr. Aberle, a member of the UCLA Health Jonsson Comprehensive Cancer Center (JCCC). “CT was shown to be the first and most effective way of reducing lung cancer mortality by virtue of early detection and potentially curative treatment.”
Yet despite an effective screening tool, few people are undergoing the procedure. According to the American Lung Association, only 5.8% of eligible Americans have been screened. For Californians, the low-dose CT screening rate plummets to 1%.
The reasons vary, but a lack of awareness is a big concern.
“Education is one of the major impediments to the diffusion of screening across the population in the U.S.,” Dr. Aberle said. “It’s not just the education of patients, it’s the education of clinicians.”
Who should be screened
In contrast to other cancer screenings, that are based on age or sex, lung cancer screening has a more complicated set of criteria, making it harder to inform both doctors and their patients about who qualifies. Additionally, as research continues, recommendations are evolving.
People are eligible for screening based on age and how much they currently smoke or smoked in the past. For people who no longer smoke, their screening eligibility also depends on how long ago they quit.
Guidelines from the U.S. Preventive Services Task Force (USPSTF), which were updated in 2021 to broaden eligibility, call for an annual screening from ages 50 to 80. A person must also have smoked for a minimum of what’s known as “20 pack-years.”
Pack-years are calculated by multiplying the number of packs of cigarettes smoked per day by the number of years an individual has smoked. For example, a person who smoked one pack of cigarettes per day for 20 years or two packs per day for 10 years would qualify.
Additionally, in order to be screened, a person who no longer smokes must have quit within the past 15 years.
Private insurance follows those guidelines for coverage. Medicare does so with the exception of the full age range, setting the upper limit at 77 instead of 80.
As is the case for some other cancer screenings, such as mammograms, there are differing guidelines. In early November, the American Cancer Society revised its recommendations to adopt the same age range and pack-years as USPSTF. (It previously recommended screening for ages 55 to 74, and with a 30 pack-year smoking history.)
However, the society now differs in one area - eligibility for former smokers. The group recommends that they should be screened regardless of how long ago they quit.
That would broaden access to more people, as those who formerly smoked have overtaken people who currently smoke.
“We are increasingly a population of former smokers, with many years since quitting,” Dr. Aberle said.
However, Dr. Aberle said the proportion of people eligible could reach unreasonably high levels, noting that the next phase in screening criteria is moving to weigh more individualized risk factors in an effort to calibrate who is most at risk.
Ashley Prosper, MD, a radiologist specializing in cardiothoracic imaging and an assistant clinical professor of radiology, said she’s also hopeful that screening eligibility can eventually be personalized.
For now, she said she’s encouraged by the American Cancer Society’s recommendation because although the risk of developing lung cancer drops substantially within five years of quitting, “the relative risk compared to those who have never smoked does not entirely go away.”
“Insurers are not mandated to follow ACS, however the ACS is a strong organization and their taking this step will likely influence our conversation going forward,” Dr. Prosper said.
Adding on another layer to getting screened for the first time, people must undergo what’s called a “shared decision-making” process to understand risks and benefits and confirm that they would be willing to undergo treatment if diagnosed with lung cancer.
Potential risks include false positive results that can lead to follow-up tests or surgery, as well as radiation exposure from having repeated screenings.
“The most significant and serious is one out of 1,000 people will undergo an unnecessary biopsy that leads to a complication like a lung collapse,” said Amy Cummings, MD, PhD, a thoracic oncologist and assistant professor of medicine.
What the test is
The low-dose CT scans can detect asymptomatic cases using one-tenth of the radiation used in a diagnostic chest CT. It produces much-higher-resolution images than a chest X-ray, Dr. Cummings said.
“It maximizes the level of detail you get with minimal radiation exposure and that’s why I think it’s so effective and has been a successful tool,” said Dr. Cummings, also a JCCC member.
To undergo the low-dose CT scan, patients lie on their backs on a scanner bed and briefly enter the “doughnut hole” of the scanner X-ray beam. They are instructed to take a deep breath to expand the lungs and hold for five to 10 seconds while high-resolution 3-D images of the lungs are captured.
“It doesn’t require contrast,” Dr. Cummings said. “The scan itself takes just a few minutes to do. I think it’s one of the more easy screenings to get done when you think about the other screenings like mammography or colonoscopy.”
The images allow radiologists to look for nodules, which are abnormal growths that can be a sign of lung cancer. A radiologist will evaluate the nodule’s features including size and density to distinguish between nodules of low and high concern.
Depending on the findings, a small number of people may need another screening sooner than in a year, Dr. Prosper said.
“The vast majority of patients that are screened have findings that we find reassuring, and stay with their annual follow-up regimen,” said Dr. Prosper, another JCCC member.
Coming back each year is important.
“The power from lung cancer screening doesn’t just come from the first scan, it comes from subsequent scans,” Dr. Cummings said. “One of the hardest things about lung nodules is knowing which is the most suspicious and the only way we see it sometimes is over time.”
If suspicious nodules or lesions are found, Dr. Prosper said, a UCLA Health multidisciplinary team of radiologists, pulmonologists and thoracic surgeons review the findings and come to a consensus on how to proceed with any necessary follow-up, such as a biopsy or PET-CT scan.
Barriers and disparities
Besides the complexity of determining eligibility, stigma over smoking also contributes to low screening rates. Some patients experience denial, guilt or feelings of unworthiness.
“One of the ways we may need to combat the disincentive for screening is by educating people and making them understand that nobody deserves to die of lung cancer,” Dr. Aberle said. “Smoking is an addiction, like many other things. There is no shame in that.”
Dr. Prosper noted that some patients aren’t comfortable admitting to their doctors that they smoke, but that UCLA Health offers comprehensive smoking cessation services.
“We also want to be your partners in smoking cessation should you be interested in quitting,” Dr. Prosper said. “We have staff who are trained in tobacco cessation counseling and therapy. We find they’re able to really support individuals through a variety of methods to help them quit.”
Screening can help address the disparities that exist when it comes to lung cancer.
“Lung cancer is the leading cause of cancer-related death worldwide,” Dr. Prosper said. “However, Black men are more likely to develop and die from lung cancer than any other group in the United States.”
She noted that the USPSTF decision two years ago to lower pack-year eligibility from 30 to 20 and to change the starting age from 55 to 50, has nearly doubled the number of Americans eligible for screening, and has increased eligibility for Black Americans, who are at risk of developing lung cancer at younger ages and lower smoking rates than the prior eligibility criteria allowed for.
Dr. Aberle said that in time screening guidelines could become more nuanced to potentially screen fewer people by targeting only those at highest risk. Such an algorithm could proportionally weigh other risk factors such as race, sex, history of chronic obstructive pulmonary disease and family history of lung cancer. Doctors in Canada and Europe have been developing such models, she said.
“Those appear to perform better,” Dr. Aberle said. “That’s a direction a lot of people are thinking about.”
For now, the UCLA Health doctors said ensuring that qualified people undergo screening is the best way to reduce cancer deaths among people at high risk.
“Nationally, only 26% of lung cancers are detected at an early stage,” Dr. Prosper said. “This is likely due to the fact that lung cancer is unlikely to cause symptoms in its early stages. Lung cancer screening enables us to find lung cancer early, before it has spread or caused symptoms.”
Courtney Perkes is the author of this article.