UCLA’s innovative and expanding menu of minimally invasive gynecologic surgery (MIGS) provides important benefits for patients: lower risks of complications, less scarring and shorter recovery times. Along with excellent outcomes, there’s another big benefit: Options.
“Historically, gynecologic surgery was done abdominally or vaginally, but over the last three decades we’ve adopted laparoscopic surgery as the ‘go-to’ for hysterectomies, removal of fibroids, ovarian cysts and more,” says Sukrant Mehta, MD, assistant clinical professor of OB-GYN and associate program director for the fellowship for MIGS.
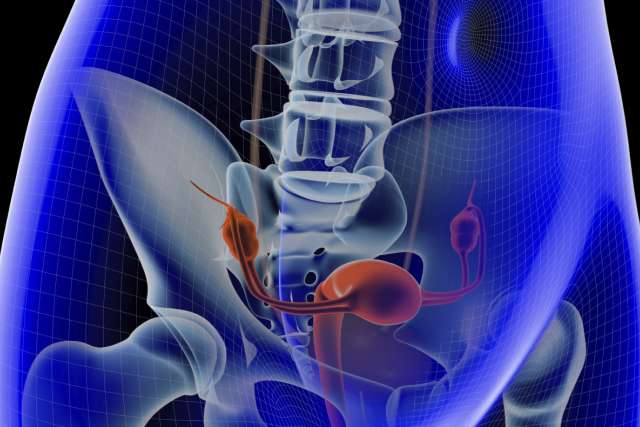
“Laparoscopy typically involves making several small incisions on the abdomen, insufflating the abdomen with carbon dioxide gas, inserting a camera and small instruments through the incisions, dissecting whatever pathology a surgeon is trying to get out of a patient and, finally, extracting it from the abdomen,” explains Dr. Mehta. Laparoscopy is the current standard of care for gynecologic surgeries.
“This minimally invasive surgery allows physicians to see everything inside the pelvis and the abdomen without having to open the patient’s abdomen with a large incision,” he adds.
Progressive new procedures, first introduced to southern California by UCLA gynecologic surgeons, have been added to that tried-and-true surgical approach. Vaginal natural orifice transluminal endoscopic surgery (vNOTES) combines the benefits of laparoscopic and vaginal surgery.
“The first time I saw it, my mind was blown,” says Dr. Mehta. “I thought, ‘Making use of a natural orifice is pure genius.’ We make an incision high in the apex of the vagina where the patient will never see it, and it’s not very painful.”
Through that incision, surgeons inflate the abdomen and pelvis and insert small portals where a camera and surgical instruments go through.
“It’s a new approach using FDA-approved instrumentation specifically for vaginal laparoscopic surgery,” explains Ram Parvataneni, MD, professor of OB-GYN and co-director of UCLA’s Fibroid Treatment Program. “Cases including hysterectomies, ovarian surgeries,cyst removal, and fallopian tube surgeries have gone very well. We’re extremely happy with the outcomes.”
Because there are no visible incisions, healing is faster than traditional laparoscopy.
Incision-free fibroid treatment
Sonata, another progressive procedure performed at UCLA, is transcervical radio-frequency ablation of fibroids, a new FDA-approved technology that gives patients relief from the symptoms of fibroid tumors without skin incisions, says Dr. Parvataneni. “That’s an incredibly important distinction,” he stresses.
“An ultrasound probe is inserted through the cervix and into the uterine cavity, allowing us to identify borders of fibroids inside the uterus,” explains Dr. Mehta. “We then use an array of needles to treat the fibroid. The fibroid tissue is heated to 105 C, higher than the boiling point of water, causing the fibroid cells to be destroyed, without affecting the surrounding normal uterine tissue.”
“Over time, the tissue gets softer and shrinks. This has a huge impact on how fibroids affect patients, which can include heavy menstrual bleeding, pelvic pain, pelvic pressure, urinary symptoms, constipation and more,” notes Dr. Mehta.
Kathryn Goldrath, MD, assistant clinical professor of OB-GYN, stresses how important advances in fibroid treatment are.
“It’s estimated about 70% of premenopausal women are diagnosed with fibroids at some point; for Black women, that risk can be upwards of 80%,” she says. “It’s an important statistic. I have a lot of patients who come to me and the first thing they say is, ‘I have fibroids, but don’t take out my uterus.’”
Historically, certain populations, including African Americans, have felt distrust toward the medical community because of the many health injustices inflicted upon them. So, new technologies and different techniques, such as this incision-free procedure, provide options attuned to patients’ preferences, Dr. Goldrath says.
“Staying on top of new options, and educating patients about them, is one of the most important ways we provide optimal care,” she says.
Dr. Parvataneni points out that vNOTES and Sonata are covered by most health plans including government payers, helping to ensure access to care.
“We want to take care of everyone,” he stresses, “and this provides opportunities for all patients to receive the best care.”
The future is now
The physicians agree when enumerating the big takeaways about vNOTES, Sonata and MIGS in general.
“With minimally invasive surgery, we’ve been able to significantly impact our patients’ outcomes because of a lower chance of infection, less bleeding, less pain, less medication, and easier and quicker recovery,” says Dr. Mehta.
Because most MIGS are performed on an outpatient basis, hospital stays are greatly reduced, says Dr. Parvataneni. “Often patients come in, have the procedure and go right home. They can get back to their normal activities much, much faster,” he says.
Dr. Mehta says that the goal is to convert most of the gynecologic laparoscopic surgeries UCLA currently performs to vNOTES in the next 10 years. Dr. Goldrath concurs, adding, “This IS the future of gynecologic surgery.”