Fluctuating levels of estrogen and progesterone are the hallmark of the menopause transition — the years leading up to cessation of menstrual periods. These hormonal changes affect every major organ system in the body, including the brain, which can contribute to increased vulnerability to anxiety and depression.
Mood changes are common during the transition known as perimenopause, with as many as four in 10 people experiencing irritability, low energy, sadness or difficulty concentrating, according to the American College of Obstetricians and Gynecologists.
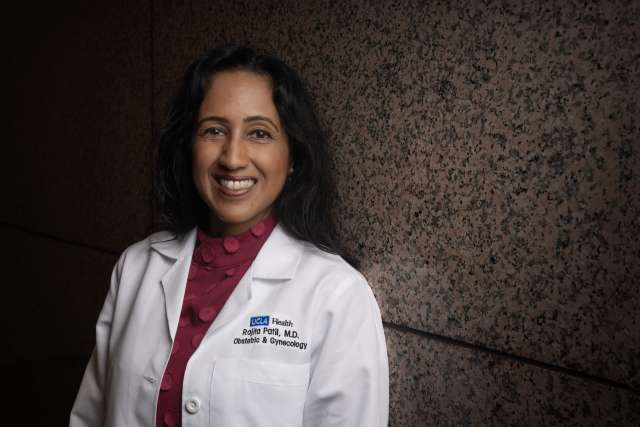
Sometimes, these mood changes can become disruptive to normal functioning because perimenopause symptoms can arise suddenly and unexpectedly, at a time in an individual’s life already often filled with responsibilities at home and at work, says Rajita Patil, MD, director of UCLA Health’s new Comprehensive Menopause Care program.
“Mood disturbance and disorders not only have a direct impact on short-term quality of life,” Dr. Patil says, “but they also increase the risk of chronic conditions such as cardiovascular disease and dementia.”
That’s why the Comprehensive Menopause Care program includes access to psychologists and psychiatrists trained in reproductive health.
Anxiety and depression
Menopause is a natural part of aging that happens to everyone with ovaries, typically around midlife. The average age is 51, but it can occur as early as 40 or as late as 60. While menopause is just a moment in time, marking 12 months without a menstrual period, the years leading up to it bring significant hormonal changes that can affect well-being both during and after the menopause transition.
Anxiety and depressive symptoms are common during this time, especially for people with a history of mental health disorders, says Katie Unverferth, MD, medical director of the Maternal Mental Health Program at UCLA Health and a collaborating physician with the Comprehensive Menopause Care program.
“People think a lot about premenstrual dysphoric disorder or PMS, PMDD. They think about pregnancy. They think about postpartum. But menopause is also a time of big hormonal transitions that can last years,” Dr. Unverferth says, adding that “it’s kind of a chaotic time from a hormonal perspective.”
It’s not just hormonal changes that contribute to mood and anxiety issues for people in menopause, notes Louise Dixon De Silva, PhD, a clinical psychologist who works with the menopause care program. A person’s feelings about aging, fertility, their place in society and other environmental-social factors also play a role.
For example, if someone is having frequent hot flashes — the most common symptom of menopause — it can have a domino effect on their life that impacts their mood, Dr. Dixon De Silva says.
“They may start to do things like avoid going to social events,” she says. “Or when they feel their face get warm, they may immediately start to get really anxious and then overthink.
“So in addition to the biological changes causing these symptoms, these symptoms change how people are engaged in their lives. And we know that when people stop seeing their friends or are having trouble at work, that also increases depression and anxiety symptoms.”
For these reasons, it is crucial to not silo the treatment of mood disturbance in menopause, Dr. Patil says, adding that the Comprehensive Menopause Care program evaluates mental health alongside sleep, hot flashes and psychosocial stressors to properly address it.
Cognitive behavioral therapy support
Dr. Dixon De Silva is leading a six-week cognitive behavioral therapy group for people experiencing vasomotor symptoms such as hot flashes and night sweats. The group will support participants in changing their thoughts about these symptoms and teach techniques for relaxation and stress reduction. Studies show that four to six sessions of cognitive behavioral therapy can significantly reduce hot flashes and improve sleep, mood and quality of life.
“A really nice perk of the group is that you are going to be around other people that are experiencing the same issues that you are and can support you in that position,” Dr. Dixon De Silva says. “These are not topics that we commonly talk about — women and aging and menopause — so gaining support is really, really important.”
Not everyone will experience mood or mental health issues during the menopause transition. But for people who do have symptoms of depression or anxiety at this time, help is available.
Cognitive behavioral therapy is an option, as well as antidepressants, which have been shown to be effective in treating depression and anxiety symptoms and improving quality of life, Dr. Unverferth says.
“Certain antidepressants can also help with hot flashes,” she adds.
Hormonal changes associated with the menopause transition can bring about a range of physical and mental symptoms, but the Comprehensive Menopause Care program is prepared to address them, Dr. Patil says.
“My vision is to provide evidence-based, comprehensive but individualized whole-person care,” she says. “It’s really about putting the power in the patient’s hands after having the right information and the right understanding of their health so that they can make the best decisions for themselves.”
Help Shape the Future of Mental Health by Joining the UCLA Mental Health Research Registry