How much does health care really cost?
UCLA researchers have for the first time described cost across an entire care process for a common condition called benign prostate hyperplasia (BPH) using time-driven activity-based costing. They found a 400 percent discrepancy between the least and most expensive ways to treat the condition.
The finding takes on even further importance as there isn’t any proven difference in outcomes between the lower and higher cost treatments, said study first author Dr. Alan Kaplan, a resident physician in the UCLA Department of Urology.
“The rising cost of health care is unsustainable, and a big part of the problem is that health systems, health care providers and policy makers have a poor understanding of how much health care really costs,” Kaplan said. “Until this is well understood, taxpayers, insurers and patients alike will continue to bear the burden of soaring health care costs.”
The one-year study appears in the March issue of Healthcare: The Journal of Delivery Science and Innovation.
In 2013, researchers from the University of Iowa called more than 100 hospitals seeking the cost of a hip replacement and found the range in price estimates was huge. In some instances, hospitals could not even provide a cost. UCLA researchers wanted to use a new technique, time-driven activity-based costing, to determine how much it costs at UCLA to take care of BPH, or enlarged prostate, which affects about half of men over 50 and can be treated in many different ways.
“We felt that if we could tackle the cost of such a complex and common condition we could use the technique to really understand cost on a larger scale,” Kaplan said. “Most importantly, we found that within our own institution the cost of treating BPH varied about 400 percent and, as of yet, we have no proof that one way is any better than the other.”
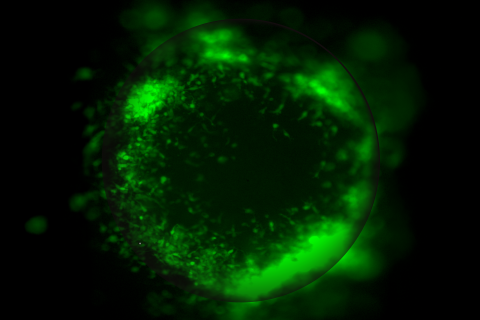
BPH can be treated medically, but invasive procedures often are needed for patients in whom medical therapies are no longer effective. These procedures range from in-office minimally invasive to outpatient surgery to inpatient open surgery to remove the majority of the prostate tissue. The pre-operative work-up varies significantly, which represents a large part of the cost differential, Kaplan said.
Time-driven activity-based costing is a novel strategy developed by Harvard Business School health care economists that estimates cost and demand through measuring the unit cost of supplying capacity and the time required to perform a transaction or an activity.
Kaplan and his team created a process maps that detailed each step of care for a BPH patient. They determined space and product costs and calculated personnel capacity cost rates. They calculated personnel costs for the BPH medical management team of doctors, nurses and patient affairs based on the steps of the process. Space and equipment costs also were defined.
“Cost can be a dirty word in medicine. People want the best health care money can buy,” Kaplan said. “A poor understanding of health care costs means a lot of waste and unnecessary expenses that are borne mostly by patients. Value in health care demands high quality care at the lowest possible cost.”
Going forward, UCLA researchers are collecting and analyzing data to determine value in BPH, including which tests add value to care and which may be unnecessary.
The study was a collaborative effort of the UCLA Department of Urology and the UCLA Institute for Innovations in Health.
According the American Urologic Association, BPH affects about 50 percent of men between 51 and 60 and up to 90 percent of men over 80. The condition is caused by the non-cancerous enlargement of the prostate gland due to aging. Symptoms include difficult and/or frequent urination, dribbling after urination and pain during urination.
“Time-driven activity-based costing can be used to measure cost across an entire care pathway in a large academic medical center,” the study states. “As financial risk is shifted toward providers, understanding the cost of care will be vital. Future work is needed to determine outcome discrepancy between the diagnostic and surgical modalities in BPH.”