Acute Pain and Regional Anesthesiology
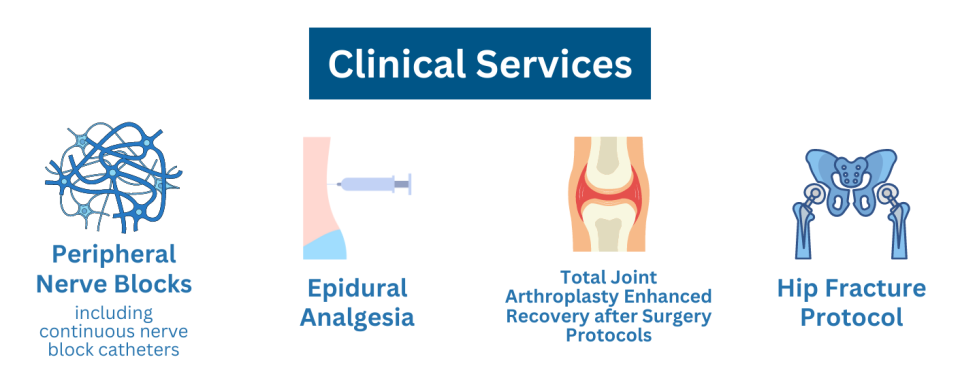
As a preeminent division of Regional Anesthesiology and Acute Pain Medicine, our mission is to deliver exceptional patient care, conduct leading research, and provide premiere education in Regional Anesthesia & Acute Pain Medicine for our trainees. Clinically, the Regional Anesthesiology and Acute Pain Service under the Department of Anesthesiology and Perioperative Medicine at UCLA is committed to facilitating recovery for our patients by offering state of the art perioperative multimodal pain management. Our goal is to employ a multifaceted approach to pain, including regional anesthesia techniques, to prevent the development of chronic pain and improve the acute pain management and functional recovery for our patients. We have specialist-driven teams located at both Ronald Reagan UCLA Medical Center and UCLA Santa Monica Hospital.
Education
We take pride in the comprehensive training we provide in Regional Anesthesiology and Acute Pain Medicine. We offer a premiere 12-month fellowship in Regional Anesthesia and Acute Pain Medicine. Fellow physicians are trained by multiple nationally-recognized faculty in Regional Anesthesia and Acute Pain Medicine and rotate through various sites, including UCLA Santa Monica Hospital, Ronald Reagan UCLA Medical Center, and several UCLA surgery centers. Upon completing fellowship, our fellow physicians are equipped to become leaders in the field and are facile with performing a variety of basic and advanced regional anesthesia procedures, experienced in running a high-volume acute pain service, and able to act as expert perioperative acute pain consultants.
Learn more about our Regional Anesthesiology and Acute Pain Medicine Fellowship
Our resident physicians obtain exposure to Regional Anesthesia and Acute Pain Medicine (RAPM) at multiple sites, each offering our resident physicians insight into RAPM best practice. In addition to learning technical procedural skills like peripheral nerve blocks and epidural anesthesia, residents gain an understanding of how to assess and manage acute postoperative pain, trauma pain, cancer-related pain and acute pain exacerbation in patients with chronic pain who need to be admitted to the hospital.
Research
Our division is continually involved in advancing the field of RAPM with an active spirit of academic exploration and inquiry. We collaborate with peer institutions on multi-center research trials, conduct locally driven clinical research, and present our work annually at regional, national, and international conferences. Our residents and fellows present at the annual meetings for ASA, CSA, ASRA, WARC and our very own UCLA Scientific Evening. Throughout all our academic efforts we aim to highlight novel ways to enhance patient outcomes within acute pain.
Leadership

Natale Z. Naim, MD
Regional Anesthesiology & Acute Pain Service, UCLA Medical Center, Santa Monica

Siamak Rahman, MD
Regional Anesthesiology & Acute Pain Service, Ronald Reagan UCLA Medical Center

Pamela A. Chia, MD, MS
Regional Anesthesiology & Acute Pain Medicine Fellowship Program

Valeria Carcamo-Cavazos, MD
Regional Anesthesiology & Acute Pain Medicine Fellowship Program
Our Team





