Post-Traumatic Stress Disorder
Responsive Neurostimulation for Post-Traumatic Stress Disorder - Principal Investigator: Jean-Philippe Langevin, MD
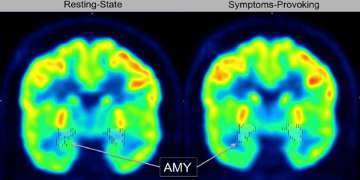
Post-traumatic stress disorder (PTSD) refractory to treatment is marked by failure of fear extinction and its biological substrate, amygdala reactivity to trauma reminders13,14. Decades of research have clarified the neuronal mechanisms coordinating fear extinction and consolidation15. Fear cells and extinction cells in the basolateral amygdala (BLA) alter their firing rate based on the nature of the stimulus and the influence from the medial prefrontal cortex (mPFC) and the ventral hippocampus (vHPC)16,17. Together, the BLA, mPFC, and the vHPC form an anxiety-processing network15,2 where the BLA links stimulus to emotion, the vHPC provides memory context, and the mPFC coordinates extinction or consolidation. Local field potential (LFP) recordings from the BLA have revealed specific signals that correspond to an enhanced fear state. We have previously shown that neuromodulation of the BLA can promote extinction in a rodent model18 and in a treatment-refractory PTSD patient19. This action is likely carried by disrupting fear signals within the BLA; however, continuous neurostimulation may also disrupt normal function of the amygdala.
The present application proposes to investigate the use of Responsive Neurostimulation (RNS, Neuropace) in six (6) veterans suffering from severe treatment-resistant PTSD. This dual-activity device will allow us to chronically record LFPs from the BLA under specific conditions such as fear conditioning, exposure to trauma reminders, and emotional memory encoding and retrieval. In addition, the neural activity will be captured during real-life symptoms of flashback and nightmares. These recordings will provide us with the specific electrophysiological biomarkers of hypervigilance and re-experiencing. The device will then be programmed to detect and treat these biomarkers with a pre-determined electrical pulse. The patients will be followed prospectively using psychological scales but also with functional neuroimaging and electroencephalograms. These modalities will be used to determine the extent of circuit engagement as a result of the therapy. By approaching PTSD from a fear processing mechanism perspective, our project will serve as a proof of concept for other circuit-based therapies in psychiatry. This proposal is a multi-departmental effort involving 11 investigators across 7 departments and requires a close collaboration between clinical and basic scientists. As a result, the findings underlying our chronic recordings will bridge the basic science results from fear conditioning research to clinical neural processes in PTSD patients.
Investigators: Jean-Philippe Langevin, MD; Avishek Adhikari, PhD; Ausaf Bari, MD, PhD; James Chen, MD; Michael Fanselow, PhD; Ralph Koek, MD; Scott Krahl, PhD; Alexis Kulick, PhD; Mark Mandelkern, MD, PhD; David McArthur, PhD; David Sultzer, MD; and Nanthia Suthana, PhD
Sponsor: NIH/NINDS ($4.2 million)
Purpose: By approaching PTSD from a fear processing mechanism perspective, our project will serve as a proof of concept for other circuit-based therapies in psychiatry. This proposal is a multi-departmental effort involving 11 investigators across 7 departments and requires a close collaboration between clinical and basic scientists. As a result, the findings underlying our chronic recordings will bridge the basic science results from fear conditioning research to clinical neural processes in PTSD patients.