Breast Lesion Localization
By: Steven Lee, MD, Fadi Dahoud, and Daniel Bradley, MD
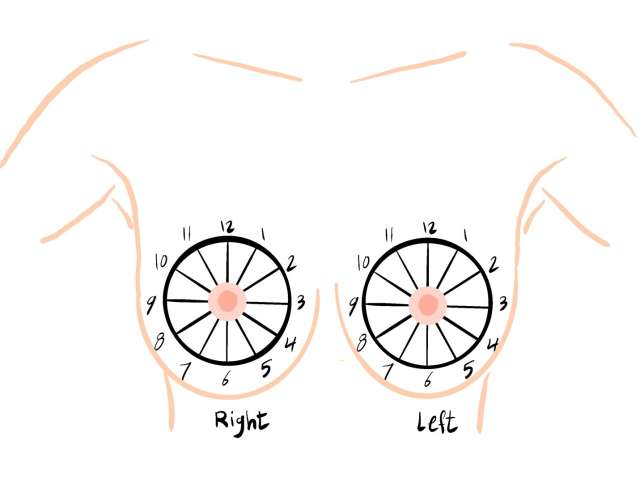
When evaluating breast findings, it is important to accurately identify their location. Findings in the breasts are described by their orientation on a clock face (Figure 1). When deciding on the clock face location of a finding on mammography two standard mammographic views are used, the MLO (mediolateral oblique) and CC (craniocaudal) views.
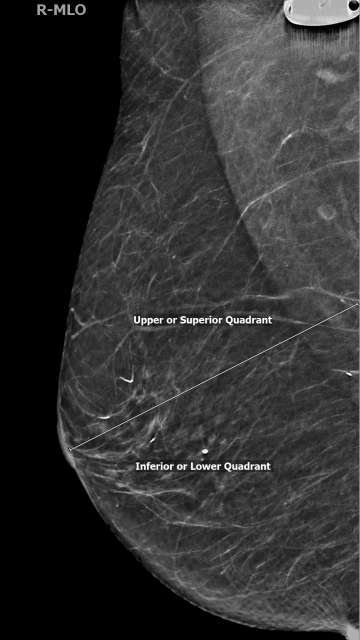
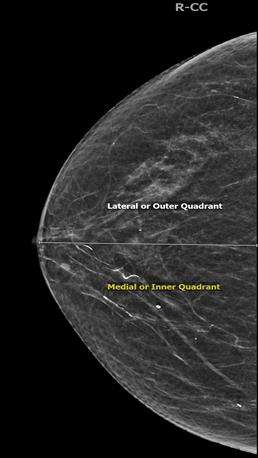
In the MLO view, lesions above the nipple are in the superior/upper quadrant while lesions below the nipple are in the inferior/lower quadrant. The superior quadrant spans from 9:00 and 3:00, while lower quadrant spans from 3:00 to 9:00 in a clockwise orientation (Figure 2). In the CC view, lesions lateral to the nipple are in the lateral/outer quadrants while lesions medial to the nipple are in the medial/inner quadrants. The lateral quadrants in the left breast span from 12:00 to 6:00, however the lateral quadrants of the right breast span from 6:00 to 12:00 (both in a clockwise orientation). Similarly, medial quadrants in the left breast span from 6:00 to 12:00, while in the right breast the medial quadrants span from 12:00 to 6:00 (Figure 3).
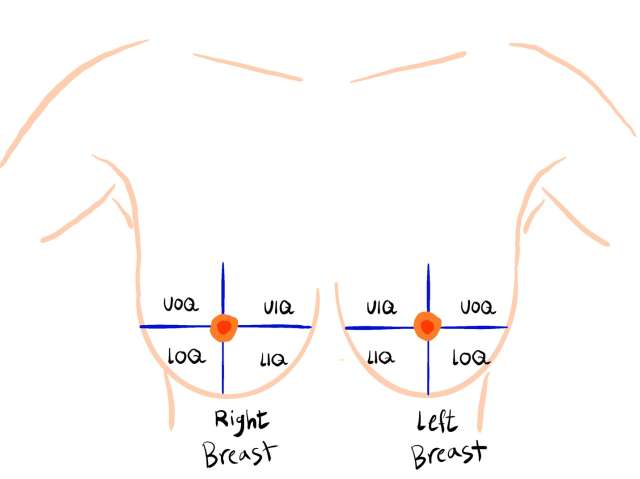
When used together, MLO and CC views can be used to localize lesions into different clock faces as detailed above and into one of four quadrants: upper outer quadrant, upper inner quadrant, lower outer quadrant and lower inner quadrant (Figure 4). Please note that the quadrants in a breast are mirror images of the quadrants in the contralateral breast.
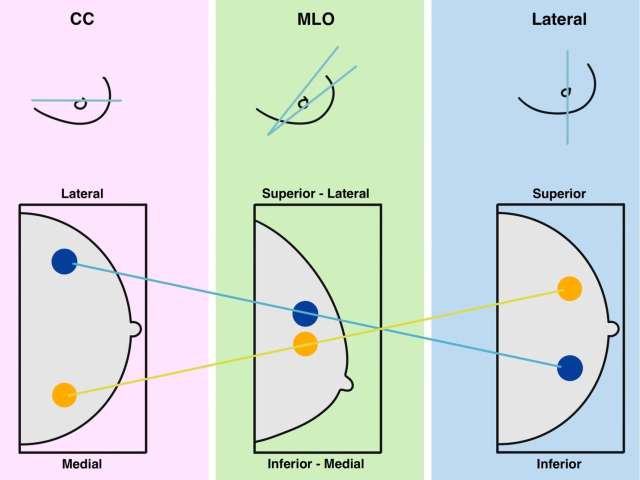
If a lesion is only seen on MLO or CC views, additional mammographic views can be obtained to further localize it. If the lesion is only seen in the MLO view, an ML (mediolateral) view can be obtained for additional evaluation. If the lesion is in a lower in position in the breast in the ML view when compared to the MLO view, then the lesion is lateral/outer quadrant. Alternatively, if the lesion is higher in position in the breast in the ML view, then the lesion is medial/inner quadrant (Figure 5).
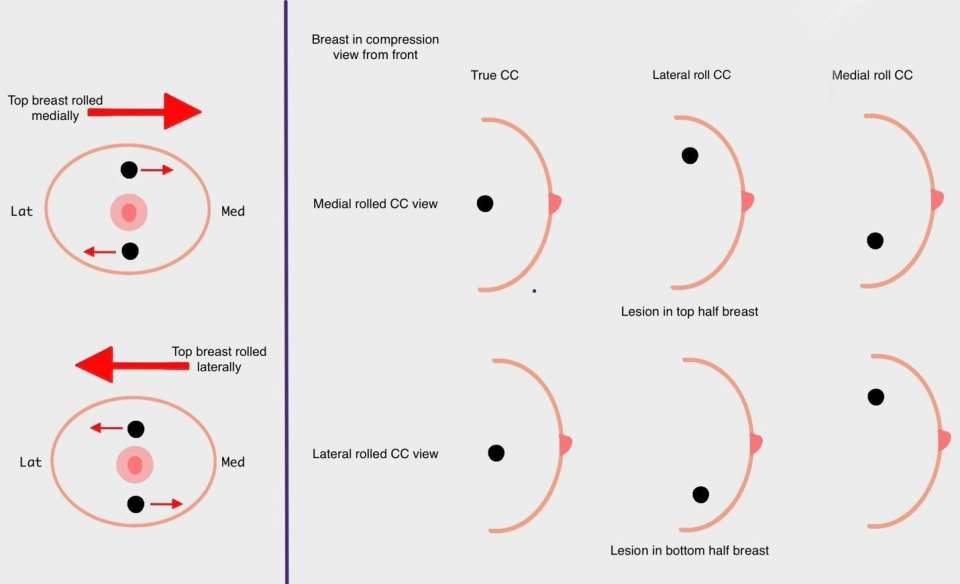
Similarly, if a lesion is only seen on CC views, rolled CC views can be obtained to aid in localization. If the superior half of the breast is rolled medially (medially rolled CC view), the lesion will be more medial in the breast when compared to its position on the true CC view if it is located in the superior half of the breast. Alternatively, if the lesion is in the inferior half of the breast, the lesion will be more lateral in the breast in the medially rolled CC view when compared to its position on the true CC view (Figure 6). A similar localization technique can be performed using laterally rolled CC views.
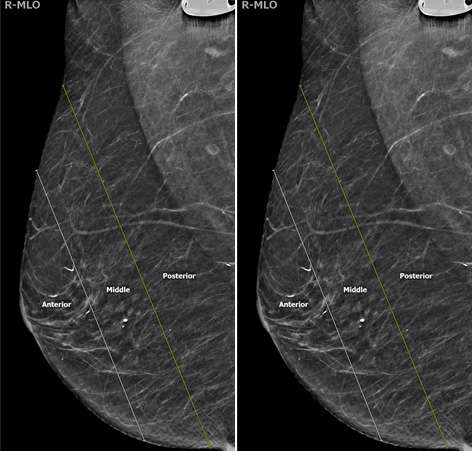
Two additional descriptors can be used to further help localize a lesion: depth within the breast and distance from the nipple. The breast is split into three layers of depth: anterior, middle, and posterior with each depth category representing approximately one-third of the breast tissue (Figure 7).
Distance from the nipple measures the distance from the lesion to the nipple to further localize the lesion on different mammographic views (Figure 8).

References
- Sun, E. X., Shi, J., & Mandell, J. (2021). Breast Imaging. In Core radiology: A visual approach to diagnostic imaging (second, pp. 592–657). essay, Cambridge University Press.
- World Health Organization (n.d.). Breast imaging – Mammography interpretation – Interpreting the abnormal mammogram. Atlas of Breast Cancer Early Detection.