Quality Improvement
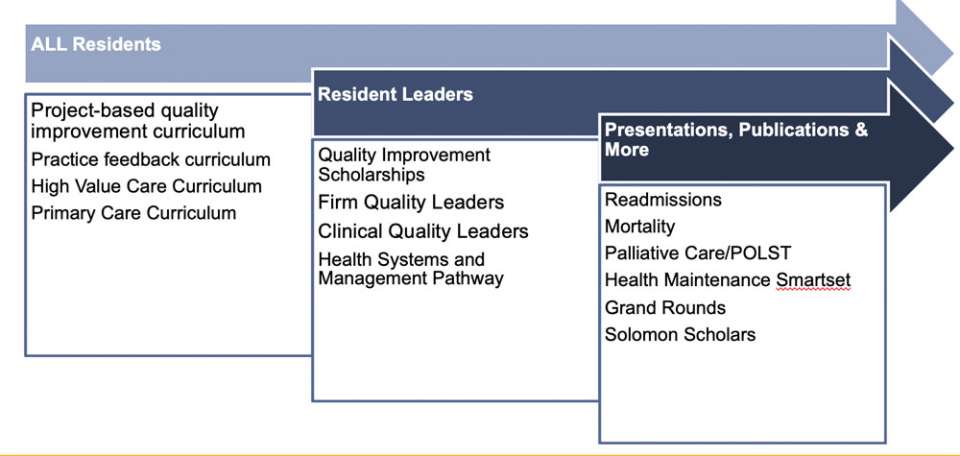
Quality improvement in healthcare is a quintessential element of outstanding care, and a great way to hold ourselves accountable that we never stagnate and constantly look for avenues of improvement. QI in medicine is now so important that it has become a common ACGME competency to apply QI methods for the goal of practice improvement. Here at UCLA, we strive to go beyond that. We are fortunate to have a robust healthcare system which values high quality care, and work closely with the larger Department of Medicine Quality Team which oversees the quality care across our inpatient and outpatient services, both teaching and non-teaching.
Our residents will complete residency with robust built-in exposure to QI in both the inpatient (Firm-based QI projects) and outpatient (clinic-based QI teaching) settings. Residents with identified interest in QI are supported by the department to apply to be a QI Scholar, with funding and pairing of a mentor in the DOM Quality Team to work on a larger health system project. Some projects our residents have done independently have improved outpatient diabetes tele-education, improved childhood vaccination rates; some projects born from our firms have streamlined bisphosphonate prescription in patients admitted with hip fractures, and improved sleep quality inpatient.
To further our culture of improvement, these initiatives by our residents are shared and published in local, regional, and national conferences and journals. We carve out dedicated time in our departmental grand rounds and residency noon conferences for our residents to share the fruits of their labor, and inspire others in the career-long path of quality improvement.
Overview
All UCLA residents are trained in quality improvement to engage and empower them to serve as agents of change in healthcare. The Department of Medicine and UCLA Health both have robust quality programs with ample opportunities for house staff involvement, education, and mentoring.
House Staff QI Curriculum and Resident-Driven QI Projects
QI Curriculum
The UCLA Internal Medicine Residency QI curriculum includes both seminar format didactics and experiential, mentored, team-based QI proposals and projects.
QI techniques taught include:
- Defining and prioritizing problems
- Assessing the current state (including the A3 format for project management)
- Writing SMART goals
- Root cause analysis (including fishbone diagrams and the 5 why’s)
- Designing and implementing solutions (including PDSA cycle/small tests of change)
- Measuring change (including selecting metrics, SPC analysis/run charts)
- Sustaining change
- A3 format for project management
All residents are involved in the selection, design, and discussion of a firm quality improvement project, and several residents from each firm have the opportunity to serve as QI leads and receive additional training, experience and mentorship.
Recent Resident-Driven QI Projects:
- Firm A: Improving patient handoffs
- Firm B: Evaluation of need of daily AM labs
- Firm C: Improving the quality of night float sign-out on the medicine wards
- Firm D: Improving the quality of post-hospital discharge instructions
- Firm E: Improving the appropriate usage of inpatient PT/OT services
Resident Practice Performance Feedback
We have developed a quality dashboard for the inpatient teaching service and outpatient resident primary care practice panels. Residents have access to group-level performance data as well as their own individual data, including peer comparison. Through a practice feedback curriculum, they are taught how to interpret this data to reflect on their own practice, identify gaps in care, and implement improvements. All housestaff therefore gain experience in practice audit and feedback, panel management, and ambulatory-based quality improvement.
Rapid Mortality Review
All housestaff participate in Rapid Mortality Review (RMR), an innovative process to conduct near real real-time, structured reviews of inpatient deaths with a multidisciplinary team of front-line providers. RMR has proven extremely effective in identifying systems issues and opportunities for improvement in end-of-life care. It has inspired a number of quality action items and had educational and humanistic value.
Housestaff QI Scholarships
In 2011, the DOM Quality Program established the Housestaff QI Scholarships, awarding 5-6 housestaff a year. These residents receive additional quality training and mentoring, design and implement a quality project and present their results at Medicine Grand Rounds. Some have also presented their work nationally and/or published.
Recent Department of Medicine Quality Scholars:
- Kalei R.J. Hosaka, Med-Peds Class of 2025
- Akshara Malla, Med-Peds Class of 2025
- Jennifer Mansour, Class of 2025
- Jacob Roberts, Class of 2025
- Sammy Sayed, Class of 2025
- Anna-Claire Siena, Primary Care Class of 2024
Safety
Residents participate in hospital quality and safety processes such as event reporting and root cause analysis of adverse outcomes. They are also involved in a number of quality initiatives targeting patient safety, such as the Safe Discharge Best Practices Pathway, standardized central line training, a three-year simulation curriculum including interdisciplinary team training, an “Inpatient Checklist” targeting CAUTI and VTE prevention, and standardized signout and handoff processes.
Value
UCLA’s residency program has an active “Physicians for Responsible Ordering (PRO)” chapter, which has organized a number of educational and value-based care improvement initiatives, such as multi-site cost-of-care case conferences and weekly feedback on lab ordering costs to wards teams. The Division of General Internal Medicine-Health Services of Research recently launched the UCLA Value Based Care Research Consortium.
UCLA Health Quality and Safety
UCLA Health is a leader in quality and safety. Housestaff can participate in a wide variety of hospital initiatives, which include reducing mortality, improving outcomes measures, value-based care redesign, enhancing the patient experience, reducing readmissions, and strengthening patient safety. Residents also participate in hospital quality and safety processes such as event reporting and root cause analysis of adverse outcomes.
The Housestaff Quality Improvement Council (HQIC) is a housestaff-led quality improvement council supported by Executive Leadership. The council provides a venue to target quality improvement issues, strengthen collaboration between departments, and provide exciting academic opportunities.
The UCLA Healthcare Improvement Institute, a collaboration between UCLA Health Operations and the Schools of Medicine and Nursing, provides quality and Lean training to providers and staff in certificate-based programs led by instructors and coaches from the Performance Excellence department.
Contacts
If you have any questions about Quality, Safety and Value in UCLA residency training, please contact Dr. Wendy Simon at [email protected].