Guidelines for Travel
Find your care
You receive customized, exceptional diabetes treatment and education in a caring environment. Call 310-825-7922 to connect with a diabetes specialist.
What to take when traveling
Bring your diabetes care items with you in a carry-on bag (not checked in a luggage compartment). Always take double the amount of supplies you think you will need.
Items below that are starred should be included in a “mini kit” that you should have readily available:
- Vials and/or pens of your long- and rapid-acting insulins*
- Insulin syringes and/or pen needles* (pack twice as many as you think you may need)
- Glucose monitoring equipment* (meter and strips) – including extra batteries
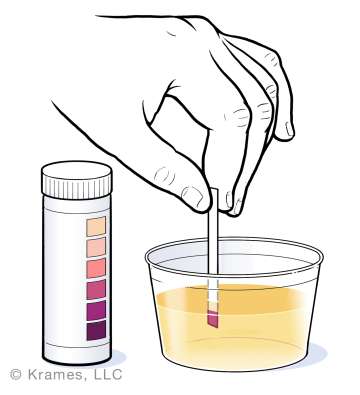
- Testing equipment for ketones (Ketostix or Precision Extra urine strips)
- Non-perishable snacks
- Glucose tablets or gel*
- Glucagon Emergency Kit
- A letter stating you have diabetes that specifies:
- Your need for daily injections and that you must carry a supply of medication and syringes
- Any allergies
- Your need for any special foods
(Note: FAA rules have changed in recent years and a letter may or may not be required.)
- Spare prescriptions for syringes and insulin with dosing instructions
- First-aid medication and supplies:
- Pepto-Bismol, Kaopectate, Imodium
- Dried soup mixes and powdered energy drinks to use if you get sick and need fluids
- Medical Identification – A bracelet or necklace stating medical diagnosis, allergies and a list of medications including insulin may be of benefit especially in a time of emergency. More information can be found at medicalert.org.
Precautions
Medication storage - Keep insulin at a temperature of 40 to 86 degrees Fahrenheit
- Do not pack insulin or medication with your luggage or in airline storage compartments. Airline storage compartments may reach temperatures below 40 degrees Fahrenheit. If insulin freezes, it will lose effectiveness (although it will not change its appearance).
- Do not store insulin in a car or trunk unless it is stored in an insulated container.
- If the weather is extreme, consider putting your insulin in an insulin cooling case.

Bring a comfortable pair of walking shoes
- Stack heels and rubber soles are more comfortable than either extremely flat shoes or shoes with slender heels. Consider wearing well-fitted sneakers/athletic shoes with cotton socks. They provide support and a soft walking surface.
Check your feet daily

- Examine your feet, especially the heels and soles, every day.
- If there is redness, apply moleskin based bandage to prevent further skin breakdown.
- Any break in the skin requires further attention.
Consider bringing or purchasing your meal before getting on the plane
- Airlines provide meals for purchase and often offer the choice to pre-order.
- Bring non-perishable snacks. Even the best of plans fail and you could end up stranded overnight in an airport or not liking the food choices that are available. Therefore, you should always have a ready source of food and medicine available. There are a variety of commercial products that travel well: blister packs of crackers and cheese, peanut butter snacks, instant cereal, etc. Consider dried soup mixes and powdered energy drinks to use if you get sick and need fluids.
If you need to avoid drinking the water
In some countries, the water may be contaminated.
- The following beverages may be safe to drink: boiled water, hot beverages (such as coffee or tea) made with boiled water, canned and bottled carbonated beverages. You can also purchase water purification bottles and pills in a travel or sport store.
- Ice may be made from unsafe water and should be avoided.
- It is safer to drink from a can or bottle of beverage than to drink from a container that may not be clean.
- In areas where water is contaminated, avoid all but bottled water – and do not brush your teeth with tap water.
- Avoid fresh fruits, fresh vegetables and salads (as these are washed in water). If you peel fruit yourself, it is generally safe.
Consult Your Health Care Provider for Specific Individual Instruction on Dosage Adjustments
Medication
Always travel with your medications in your carry-on bag. Bring a written list of all prescribed medications in the event that you lose your medications during travel. If you are taking basal insulin one or two times per day, please consult your diabetes team for instructions on how to adjust to a new time zone.
Insulin Pumps (please refer to Insulin Pump Travel Tips section)
There have been reports of bubbles entering the system and unintended boluses occurring during airline descent and ascent. It is recommended you contact your pump manufacturer for specific directions for your pump, or disconnect prior to ascent and descent and inspect tubing and reservoir. Any visible bubbles in the system should be removed prior to reconnecting the device.
Safety tips
Learn how to obtain medical assistance in an emergency
- Learn enough of the language to request help.
- Hotels in every country have access to English-speaking doctors. Many credit cards have an emergency service that will provide you with the names of English-speaking doctors in many foreign countries.
- Call the U.S. Embassy or the Consulate for additional listings.
- Alert travel companions of the possibility of a low blood glucose. Teach them the signs and symptoms of low blood glucose and give them specific instructions for treating it if you are unable to do it yourself. Teach them how and when to administer glucagon.
Consider what impact you might experience from hot tubs/whirlpool, sauna or thermal baths
- Check with your diabetes team to see if you can safely use a hot tub or sauna. Individuals with neuropathy, heart disease, circulation problems, high blood pressure, and skin infections are at higher risk for complications.
- Both dry and moist heat increases blood flow to your skin and is likely to affect the action of your insulin. You might experience lower blood glucose.
- Intense heat causes you to lose fluids and a fall in your blood pressure is possible. Be sure to drink plenty of fluids before and after using a hot tub or sauna.
- People with neuropathy are less sensitive to heat and are at increased risk for burns.
Determine if you need special immunizations
- Obtain any immunizations needed at least one month before you leave. If they make you ill or you experience side effects, you’ll have time to recover before the trip.
- To find out if you need immunizations, contact the CDC for information:
404-332-4555 or cdc.gov/travel or refer to The Yellow Book: Health Information for International Travel (an in-depth travel reference book published biennially by the CDC).
Traveling with diabetes requires extra planning even before you leave home. Certain precautions should be taken to assure a safe and healthy trip. Changing meal times, types of food, activity levels and especially changing time zones may upset your diabetes control. It is important to be prepared for potential issues that may arise and to be equipped with the tools to solve them.
Preparing to travel
- Make an appointment with your endocrinologist or diabetes educator one month prior to your travel date. Bring your flight information and be prepared to discuss dosing and timing of insulins for travel, troubleshooting your pump, the type of activity you expect and any dietary concerns.
- Learn how to update the time on your insulin pump device and your glucose meter prior to leaving on your trip. There is a website address and -800 customer service number on the back of your pump and glucose meter. Most companies have user guides online. Wait until the day of travel to change the time on your pump and meter and ask your health care provider about the best time to change the time on your device during the travel day. It is most important to change the time on your insulin pump to be sure the basal rates and bolus settings match up to your meal and sleep times.
- For cruises, long distance, or international travel, many manufactures have travel loaner programs. Contact your pump manufacturer at least one month in advance to apply for a loaner.
- Check with your insurance plan to see if you’re covered for getting more supplies in advance or for medical care abroad, when on long trips. If you’re thinking of studying abroad or traveling on a long trip abroad, check with your insurance plan to see if you will be covered. Also, check with pharmacies in the country you’re visiting to make sure they have the medical supplies you need.
- Educate your travel companions. Alert your companions that you have diabetes and the possibility of low blood glucose or pump problems. Teach them the signs and symptoms of low blood glucose and give them specific instructions for treatment. Review how and when to administer glucagon. During the trip, store glucagon and glucose tablets so they are easily accessible to you and your companions. Consider teaching them how to disconnect your pump, operate some basic pump functions and where to find emergency contact numbers. Ask your travel companion to carry a portion of your pump/insulin supplies and rapid-acting glucose tabs or gel.
- Learn how to obtain medical assistance in an emergency. Learn enough of the language to request help. Major hotels in every country have access to English-speaking doctors. Many credit cards have services that will provide you with the name of English-speaking doctors. Call the U.S. embassy or the consulate for additional listings.
- Consider bringing material that describes the pump (user manual, etc.). If you have not already done so, put a label on your pump that identifies it as an insulin infusion system. If you are traveling outside the country, call your pump company and request a list of foreign distributors. Shipping supplies outside the country is complicated by customs and shipping problems.
Travel checklist
Be sure to travel with plenty of supplies just in case you use more than expected, get stranded, or your trip gets extended. In addition to your personal items and clothes, you'll need to pack a "survival kit.” Carry it with you – not checked in a luggage compartment.
- Pump manufacturer customer service number
- Extra insulin vials (long- and rapid-acting) with a current prescription
- Insulin vial or pens for backup dosing (long- and short-acting insulins) in case of pump malfunction or failure
- Backup insulin schedule – a plan for giving backup long-acting and rapid-acting insulin in case of pump failure/malfunction (Discuss with your provider before the trip.)
- Insulin pump reservoirs
- Insulin pump infusion sets
- Insertion device for infusion sets
- Continuous glucose monitoring supplies – sensors, insertion device, chargers
- Tapes and adhesives
- A letter stating you have diabetes. It should specify your need for continuous insulin pump therapy and daily injections, noting that you must carry a supply of medication and syringes, and specify that you may need to have food and medication to treat/prevent hypoglycemia. Some manufacturers offer an “Airport Information Card” to carry while traveling that explains you are on an insulin pump. It is useful in the event of loss of consciousness.
- Pump user guide
- A document that states current pump/CGM settings, pump serial number and model/make number, manufacturer customer service number
- Insulin storage cooler – Do not store insulin in a car or trunk unless it is kept in an insulated container. If the weather is extreme, consider placing your extra insulin in an insulated cooling case.
Airport security
Taking an insulin pump through airport security is quite common. Consider informing airport security that you have diabetes, are wearing an insulin pump and carrying supplies. Be prepared to show security agents your airport card or a letter from your doctor stating you must wear an insulin pump and carry glucose and food with you at all times.
You can continue to wear your insulin pump and/or continuous glucose monitor (CGM) while going through common security systems such as an airport metal detector as it will not harm the device or trigger an alarm. You need to remove your insulin pump and CGM (sensor and transmitter) while going through an airport body scanner. If you do not wish to remove your devices, you may request an alternative pat-down screening. Some pumps have not been tested for exposure to X-rays, including body imaging scanners and airport luggage X-ray machines. Do not send the devices through the X-ray machine. Some manufacturers recommend disconnecting at your infusion site prior to security checkpoints.
If you encounter any difficulty when trying to pass through airport security, ask to speak with the TSA ground security commissioner or the international equivalent. Travel rules are subject to change so it is advisable to check with the Transportation Security Administration (TSA).
Equipment interference in flight
The Federal Aviation Administration (FAA) requires that devices with radio frequency capabilities not be used on an aircraft. Check with the TSA. International passengers should consult their individual air carriers for international regulations for insulin pumps, personal CGM and security.
Fluctuations in glucose on travel days
Fluctuations in glucose are common during travel. Test your glucose more frequently on travel days. Be prepared for low and high blood glucose during travel as the changes in time zone, meal schedule, diet, physical activity and increases in stress or excitement can alter your blood glucose. Carry backup insulin, glucagon and supplies with you on board. Wear your medical alert ID bracelet or necklace that states you have diabetes and are on an insulin pump.
Insulin dose and time settings
It's hard to predict how each individual may respond to travel. Increased activity associated with sightseeing, etc., may lower your blood glucose while a change in usual meals may increase blood glucose. The best way to decide the need for a change while vacationing is to check your blood glucose more frequently and base decisions on results.
Here are some guidelines to decide which insulin is affecting the blood glucose:
- The fasting blood glucose is affected by the overnight basal insulin or long-acting insulin dose.
- Blood glucose 2 hours after the meal are affected by the bolus dose taken before that meal.
- The blood glucose before lunch, supper and bedtime are affected by the daytime basal or long-acting insulin dose.
Pump failure and preventing DKA
If the blood glucose is unexpectedly increased, assume that the pump or the pump system may have failed to deliver insulin into your body. If the body goes without insulin, pump failure can lead to diabetic ketoacidosis (DKA), a life-threatening condition. Prompt troubleshooting of the pump is paramount. This may be a hardware issue or the infusion site may have been kinked, clogged, or pulled out. Less frequently, it is spoiled insulin or a software or mechanical problem in the pump.
If you have an unexpected high blood glucose over 250 mg/dl, after recently changing your infusion site, or when no food was eaten or 2 to 4 hours after giving insulin and you are remaining elevated, take action promptly:
- Immediately examine and inspect the site, tubing, syringe/reservoir and the pump.
- Take an injection of insulin by traditional vial and syringe (or insulin pen if available), as per your pump back up plan.
- Replace the pump syringe/reservoir, the entire tubing and cannula, and place the infusion set in a different location.
- Monitor blood glucose levels and urinary ketones closely (every 1-2 hours) any time there is concern about your blood glucose.
- If ketones are positive, this is a good indication that you have not received insulin through your pump for many hours – and you are at risk for (or in) DKA, which can cause critical health problems and may require immediate medical attention.
- If your pump or site has failed, it is recommended to call your diabetes provider immediately to discuss an action plan for safety.
Changes in time zones
It is important to remember that you always need insulin – whether you plan to sleep, exercise, or eat. It is hard to predict the exact effect that changing time zones will have on your blood glucose. If you are traveling to a time zone that is more than 1 hour different than your current time zone, it is recommended to adjust the timing of your pump.
- If the time zone changes are less than 2 hours, you simply change the time on your pump when you arrive at your destination.
- If the time zone changes exceed 2 hours, then you should plan to adjust the time on the pump in stages. The timing of your basal delivery must be altered to accommodate the changes in your circadian rhythm that result from travel across time zones.
- Keep to local time the day you are traveling.
- The first day at your destination (usually in the evening), change the time on your pump or giving long-acting insulin by 2 hours.
- The second day at your destination, change the pump time by another 2 hours.
- Continue to do this adjustment daily until the time on your pump matches local time.
- Repeat the above procedure for your trip home.
- Consult your diabetes provider for a full set of recommendations.
Traveling westbound
The main risk is hyperglycemia (high blood glucose) when a traveler gains 3-5 hours, and a delay in the dose of basal insulin can cause highs or even ketosis. If you are on NPH or mixed insulin, your risks are even greater. Consult your provider prior to travel in order to prevent complications.
If you take long-acting insulin in the evening:
- Keep the time that you take your long-acting insulin the same.
(Example: If traveling to California from New York, you would continue to take the long-acting insulin at 11 pm New York time, which would be 8 pm California time.)
If you take long-acting insulin in the morning:
- If you choose to take your long-acting insulin at your usual time, this would mean taking the insulin in the middle of the night at your destination (Example: 7 am New York time = 4 am California time.)
- You may want to gradually change the timing of your dose so that you would be taking the insulin in the morning at your travel destination. To do this, move the injection time back by 2 hours every day until the dose is given at your target time at the destination:
- Keep to local time the day you are traveling and take the morning insulin dose at your usual time. For the next day, plan to move the usual injection time “backward” or 2 hours earlier.
- On the first day at your destination, take your insulin dose at the "adjusted morning time.” After you take this dose of insulin, move your injection time back again by another 2 hours.
- On the subsequent days at your destination, continue to adjust the timing of your dose by 2 hours until the time you usually take your dose matches local time.
- Repeat the above procedure for your trip home.
If you are on NPH twice per day, consult with your doctor because a correction scale of rapid-acting insulin may be recommended to avoid hyperglycemia that may occur during westward travel.
Premixed insulins are discouraged for traveling time zones since titration is difficult.
People with type 1 diabetes are at greatest risk for diabetic ketoacidosis during travel and need to be sure that they have long-acting or basal insulin active in their body at all times and to test frequently during times of travel.
Traveling eastbound
The danger of eastbound travel is in taking doses of insulin too early and having a shortened day, causing low blood glucose levels. Some providers may want to reduce doses of long-acting insulins proportional to the hours lost. You may consider the following:
If you take long-acting insulin in the evening:
- You can choose to take the insulin at your usual time but this would mean taking the insulin in the middle of the night. (Example: 11 pm New York time = 4 am Paris time)
- An alternative is to gradually change the time of your dose so that you would be taking the insulin in the evening at your destination. To do this option, you will move the injection time ahead by 2 hours every day until the dose is given at the target evening time at the destination:
- On the day you are traveling, move your injection time ahead by 2 hours and take the long-acting insulin dose at that “adjusted evening time.” After you take this dose, adjust the next injection time forward by 2 hours.
- The first day at your destination, take your insulin dose at the "adjusted evening time.” After you take this dose of insulin, change your insulin dose timing again by another 2 hours.
- On the subsequent days, continue to adjust your insulin dose timing by 2 hours until the timing of your injection matches local time. You can then take your evening dose at the usual time.
- Repeat the above procedure for your trip home.
- Another option is to split the dose of long-acting insulin and take it 12 hours apart.
If you take SOME of your long-acting insulin in the morning:
- On the day of travel, the dose of insulin you take in the morning remains the same.
- The dose of long-acting insulin that you would be taking on the plane the first morning at your destination should NOT be taken. Instead, at the lunch meal on that day, take half of your usual dose.
- The second day at your destination, resume taking your usual dose in the morning.
Store insulin in a cool and dry place, 40-86 degrees, and avoid direct sunlight exposure. If insulin is exposed to temperatures above or below these levels, it will lose its strength and may become ineffective. You may need a cold pack if you are camping or spending long periods outdoors. If you are on a pump and you are in temperatures over 86 degrees, your insulin will need to be changed every evening, or ask your provider about going off of your pump for the days you spend in the heat.