Hypoglycemia
Find your care
You receive customized, exceptional diabetes treatment and education in a caring environment. Call 310-825-7922 to connect with a diabetes specialist.
Have you been feeling shaky, sweaty, disoriented due to low blood glucose? Hypoglycemia, or low blood glucose, is defined by glucose levels dropping below 70 mg/dl. Immediate treatment with rapid-acting carbohydrates is essential, as hypoglycemia can be dangerous.
The following are possible reasons for hypoglycemia. If you are experiencing low blood glucose levels, contact your provider to review future methods for prevention.
Insulin

Taking too much insulin is the most common reason for hypoglycemia.
Factor: Basal (background) insulin
Includes long-acting insulins or insulin delivered via basal rate on an insulin pump.
How it lowers blood glucose
This insulin is designed to cover “background” blood glucose that the liver releases into the blood stream. It is not meant to lower blood glucose. Its job is keep blood glucose from rising when you are not eating. This insulin is also not meant to cover the rise in blood glucose from food. If you did not eat, and did not take any bolus insulin, your blood glucose should not fluctuate more than about 30 mg/dl.
If your hypoglycemia is occurring overnight, when you wake up in the morning, or prolonged periods without eating – you may be taking too much basal insulin.
What you can do
Test your basal insulin by checking blood glucose when you have not eaten or bolused with insulin for at least 4 hours.
Check blood glucose every hour. Your blood glucose should stay within 30 mg/dl of your starting blood glucose. If your blood glucose drops more than 30 mg/dl during this test, you may have too much basal insulin. If your blood glucose rises more than 30 mg/dl during this test, you may have too little basal insulin.
The test is typically repeated to ensure accurate findings. Discuss with your provider and/or educator.
Factor: Bolus (mealtime) insulin
Includes rapid-acting insulin given before meals or insulin delivered as a meal bolus with insulin pumps.
How it lowers blood glucose
This is insulin designed to prevent the rise in blood glucose due to carbohydrates ingested in a meal.
If hypoglycemia occurs within approximately 4 hours after eating, you may have taken too much bolus insulin.
What you can do
If you are taking a fixed dose of insulin before meals, discuss this with your doctor, and review the information in the “food” section.
If you use an insulin-to-carbohydrate ratio (ICR), test this ratio via the following steps. Check your pre-meal blood glucose. If you do not plan to add a correction dose, eat a meal with accurately counted carbohydrates. Choose foods that have labels and are easy to measure. If 4 hours later, your blood glucose is more than 30 mg/dl below or above your pre-meal blood glucose, your ICR may need to be adjusted. Repeat this test 2-3 times and discuss with your diabetes team.
Factor: Bolus (correction) insulin
Includes rapid-acting insulin given to correct high blood glucose or insulin delivered as a correction bolus via an insulin pump.
How it lowers blood glucose
This insulin is designed to lower high blood glucose. It is usually added to the meal bolus but can also be taken when not eating, as long as there is no “insulin on board” (insulin from a previous bolus still working to lower blood glucose).
If hypoglycemia occurs within approximately 4 hours of taking a correction bolus, you may have taken too much correction bolus insulin.
What you can do
If you are using a sliding scale to add correctional insulin to your meal bolus, discuss this with your doctor.
If you use a correction factor (CF), also called insulin sensitivity factor (ISF), test this factor via the following steps. Start the test when your pre-meal blood glucose is high, and you have had no food or bolus insulin for 4 hours. Skip the meal, but take your correction bolus. Check your blood glucose every 1-2 hours for 4 hours. If 4 hours later, your blood glucose is more than 30 mg/dl above or below your target, your CF may need to be adjusted. Repeat this test 2-3 times and discuss with your diabetes team.
Factor: Giving several correction boluses too close to each other. This is called “insulin stacking.”
How it lowers blood glucose
Rapid-acting insulin remains active for approximately 4 hours. If your blood glucose is high within 4 hours of taking bolus insulin, and you take more insulin to try and lower the blood glucose, this can put you at risk for hypoglycemia due to stacking because now there is too much insulin in the system.
NOTE: Insulin stacking occurs when you take too many correction boluses without considering “insulin on board.” If you eat more carbohydrate, you need to take another bolus to cover the food.
What you can do
Consider “insulin on board” before taking another bolus to correct high blood glucose. About half of a rapid-acting insulin bolus is depleted after approximately 2 hours. The other half of the bolus gradually decreases over the next 2-4 hours. Discuss how to avoid hypoglycemia from insulin stacking with your diabetes team.
If on a pump, your pump will calculate the “insulin on board” and subtract it from your correction bolus. Discuss the proper pump settings for your insulin action time with your diabetes team as this will also impact your “insulin on board.”
If you are on insulin pens or vials, recording your insulin doses in your continuous glucose monitoring app or in a logbook will help remember the time you gave the last insulin dose. Apps such as Rapid Calc or Diabetes 360 can help you calculate your insulin dose by taking the “insulin on board” into consideration. “Smart” pens may also assist in calculating “insulin on board” and reduce stacking. Consult your diabetes team for the proper settings.
Food
Food, and in particular carbohydrates, raise blood glucose. Taking too much insulin for carbohydrates you eat can lead to hypoglycemia.
Factor: Not eating enough carbohydrates at your meal
How it lowers blood glucose
This can cause hypoglycemia if you take a fixed dose of insulin. A fixed dose of insulin will require you to eat a fixed amount of carbohydrate at your meals. If you eat fewer carbohydrates, you may have hypoglycemia.
What you can do
Accurately count carbohydrates. Measure food, read labels, and use carb-counting apps such as Calorie King, My Fitness Pal or Lose It.
If you want more flexibility in your food choices and carbohydrate amounts, talk to your health care team about using an insulin-to-carbohydrate ratio (ICR) to dose your mealtime insulin.
Factor: Inaccurately counting carbohydrates
How it lowers blood glucose
If you have hypoglycemia within approximately 4 hours of eating your meal, you may have taken too much bolus insulin for the amount of carbohydrate in the meal you ate.
This could be the result of under-estimating carbohydrates at the meal or an inaccurate insulin-to-carbohydrate ratio (ICR).
What you can do
Accurately count carbohydrates. Measure food, read labels, and use carb-counting apps such as Calorie King, My Fitness Pal or Lose It.
If you are not sure of carbohydrate content in the food, check your blood glucose frequently after the meal and be prepared to consume additional carbohydrates if you are near or within hypoglycemic levels. If you wear a continuous glucose monitor, you can monitor trends and take additional carbohydrates as needed.
Factor: Eating fewer carbohydrates than anticipated
How it lowers blood glucose
At times, you may not actually eat the amount of carbohydrates you had planned to consume. This may result in low blood glucose because you have already taken insulin to cover a certain amount of carbohydrates.
What you can do
If you eat less than expected, make up the “missing” grams of carbohydrate. If your glucose is near low or low, consider eating a food such as fresh fruit, juice or some other type of simple sugar to quickly raise glucose.
Factor: Delayed eating after taking mealtime insulin
How it lowers blood glucose
It is not uncommon to anticipate eating a meal at a certain time, take your insulin and experience a delay in eating. This is particularly true when going out to eat at a restaurant or when you have young kids.
What you can do
- Set a 10-15 minute timer after taking your meal time insulin to make sure you eat by that time.
- When at a restaurant or being served a meal by someone else, wait to give your insulin until the food is served to you.
- If insulin has already been injected, you may need to eat simple sugars to prevent your blood glucose from going too low before you start your meal. You may need to later cover that additional carbohydrate or count it as part of the total carbohydrates you ate.
Factor: High-fiber/high-fat foods
How it lowers blood glucose
Some foods, such as high-fiber or high-fat foods, may raise the blood glucose more slowly. Taking rapid-acting insulin too early when you eat these types of food may cause early hypoglycemia, because the insulin is lowering your blood glucose before the food raises it.
What you can do
If you notice low blood glucose shortly after eating these types of foods, discuss with your diabetes care team how to time your insulin when eating these foods. You may need to take your insulin shortly after the start of the meal or change the type of bolus.
Activity
Activity increases insulin sensitivity and can lead to hypoglycemia.
Factor: Light exercise
How it lowers blood glucose
Light activity can have a surprising glucose-lowering effect – from 1 mg/dl per minute up to 2-3 mg/dl per minute, depending on timing of the last insulin dose and food consumed.
What you can do
Check blood glucose before and after exercise to establish a pattern. If you use a continuous glucose monitoring device, follow the trends.
Discuss with your team tips to keep blood glucose stable while exercising. You will need to consider timing of last insulin dose, type and length of exercise, and carbohydrates consumed prior to and during exercise.
Factor: High-intensity and moderate exercise
How it lowers blood glucose
High-intensity exercise, (e.g., sprinting or weight lifting) can sometimes raise blood glucose to start. This stems from the adrenaline response, which tells the body to release stored glucose. This most typically occurs when exercising in the morning on an empty stomach.
After the initial adrenaline response, however, high-intensity exercise can drop blood glucose very rapidly (2-3 mg/dl per minute), especially if you have insulin on board from a recent bolus.
What you can do
The best way to see how individual exercise sessions affect your blood glucose is to test prior to, during and after activity, and to use a continuous glucose monitoring device to observe the effect while exercising.
You may need to lower the amount of insulin you take in the meal prior to exercise; decrease your basal rate before and during exercise (if on a pump), or consume carbohydrates before and/or during exercise. Discuss with your diabetes team prior to make any adjustments to your regimen.
Factor: Increased physical activity
How it lovers blood glucose
Increased physical activity such as gardening, house cleaning, packing, playing with the kids, walking the dog, dancing, or shopping may cause low blood glucose similar to light activity described previously.
What you can do
During such activities, check blood glucose before and after to establish a pattern. If you use a continuous glucose monitoring device, follow the trends. Treatment and prevention is similar to exercise.
Alcohol
Factor: Alcohol
How it lowers blood glucose
Under normal physiologic circumstances, the liver releases glucose to maintain blood glucose levels in the body. When alcohol is consumed, the liver is busy breaking the alcohol down. The liver, in turn, reduces its output of glucose into the bloodstream. This can lead to a drop of blood glucose levels.
It is also important to note that alcoholic drinks with carbohydrate-rich mixers (e.g., orange juice) can also raise blood glucose early with subsequent drops in glucose.
What you can do
Do not drink alcohol on an empty stomach. Always have at least a snack that includes carbohydrates.
Check your blood glucose often, especially at bedtime if you had a drink in the evening. You may need to have a snack before going to bed to reduce the risk of hypoglycemia overnight.
Have someone responsible nearby who may be able to assist with treatment of low glucose. Drink in moderation. The more you drink, the higher the risk of hypoglycemia. Consider wearing a medical alert ID before leaving home. Consult your provider for a full set of recommendations.
Treating Low Blood Glucose (Hypoglycemia)
If you are feeling symptoms such as sweating, shaking, dizziness, extreme hunger, check your blood glucose.
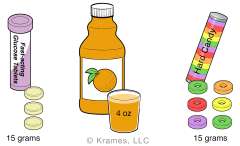
If your blood glucose is too low (below 70 mg/dL) remember the Rule of 15’s:
- Eat/drink 15 grams of fast-acting carbohydrates. Examples include:
- ½ cup (4 oz.) fruit juice
- 3-4 glucose tablets (or dextrose tablets)
- 5-6 oz. (about ½ can) regular soda, such as regular Coke or Sprite
- 8 regular Life Savers (NOT sugar free)
- 1 tablespoon sugar, honey, or jam
- Rest for 15 minutes, then re-check your blood glucose.
- If your glucose is still low, repeat Step #1
- Continue until blood glucose is over 100 mg/dL
-
If your next meal is more than an hour away, consider eating a snack with carbohydrate and protein or fat to keep your blood glucose from dropping again. Examples include:
- ½ sandwich
- Crackers with cheese
- If you can’t explain why your blood glucose was low, call your health care provider as your medication may need to be adjusted.
- Always carry fast-acting carbohydrates (simple sugar) to treat a low blood glucose.