Treatment
Find your care
You receive customized, exceptional diabetes treatment and education in a caring environment. Call 310-825-7922 to connect with a diabetes specialist.
Treatment with Insulin
Insulin introduction

Advanced insulin dosing or a basal/bolus insulin regimen is an individualized way of taking insulin. It is designed to mimic the natural secretion pattern of insulin by the pancreas. Compared to older regimens, it can improve diabetes control by minimizing wide fluctuations in blood glucose levels after meals while also offering more flexibility and safety for patients. It consists of two parts - basal and bolus insulin.
Insulin kinetics (the peak of activity and how long it lasts) vary from person to person and are dependent on factors such as dosage, site of injection, physical activity and mixing techniques. Onset, peak and duration are approximate. Exact kinetics should be reviewed with your provider.
Basal Insulin
A background dose of insulin that mostly stays constant over a 24-hour period, maintaining blood glucose levels between meals and overnight. This generally comprises 40%-60% of your total daily insulin dose but may vary depending on the individual. Commonly used basal insulins include Glargine (Lantus, Basaglar, Semglee, Toujeo); Detemir (Levemir); Degludec (Tresiba); and NPH. These insulins are typically given once or twice daily.
- Intermediate acting insulin – Insulin NPH (Humulin N, Novolin N)
Onset 1 to 2 hours
Peak 4 to 8 hours
Duration 10 to 18 hours
- Long acting (basal) insulin - Insulin glargine (Lantus, Basaglar, Semglee, Toujeo), detemir (Levemir), degludec (Tresiba)
Onset 1 to 2 hours
Peak relatively flat (dose dependent)
Duration 18-42 hours (dose and insulin type dependent)
Bolus insulin
This is a short-acting insulin typically given about 10-15 minutes before meals. It peaks 1-2 hours after administration and lasts 4 hours on average. This insulin is used to prevent rise in blood glucose due to carbohydrates in the meal (mealtime insulin) and to help lower blood glucose if it is above target range (correction dose of insulin). Examples of commonly used bolus insulins include Aspart (Novolog); fast-acting insulin Aspart (Fiasp); Glulisine (Apidra); Lispro (Admelog, Humalog); Lispro-AABC (Lyumjev); and regular insulin. Regular insulin is another form of bolus insulin but works slightly differently than above mentioned types of bolus insulins. It takes longer to work and lasts longer in the body after being injected.
- Rapid acting insulin - insulin aspart (Novolog), insulin lispro (Humalog, Admelog), insulin glulisine (Apidra)
Onset 5 to 15 minutes
Peak 1 to 2 hours
Duration 4 to 6 hours
- Short acting insulin – Insulin Regular (Humulin R, Novolin R)
Onset 30 to 60 minutes
Peak 2 to 4 hours
Duration 6 to 10 hours
Calculating your Bolus dose:
- Insulin given at meals or snacks is typically dosed by an insulin-to-carbohydrate ratio (ICR). This ensures a more accurate and precise delivery of insulin for the carbohydrates to be consumed in a meal.
- The ICR is a calculation of units of short- or rapid-acting insulin needed to cover the rise in blood glucose from carbohydrates to be consumed. For many who are newly diagnosed, the ratio provided is just a starting point. It requires evaluation by monitoring of blood glucose approximately 2-4 hours after meals, and adjusted as needed. The carbohydrate ratio may vary depending on the time of the day.
- To Calculate the Meal/Carbohydrate Dose:
- Count the amount of total carbohydrates (in grams) using your food lists, smart phone “apps” and food labels.
- Divide the total carbohydrate amount by your carb ratio to get your meal dose.
- Example: You plan to eat 60 grams of carbohydrates. Your carb ratio is 1 unit for 15 grams of carb (1:15 g). 60 grams ÷ 15 = 4 units of insulin for your food (A)
- The correction factor (CF), also referred to as insulin sensitivity factor, is used to correct (or lower) a high blood glucose down to target range.
- In order to use this, patient and their diabetes team will first establish a target blood glucose. The correction factor is only used when the blood glucose is above pre-decided target. Initially, it is also an estimate, which may need to be evaluated and adjusted. The timing of correction dosing is also important and usually provided pre-meal or at least two hours after the last bolus.
- To Calculate Correction Dose:
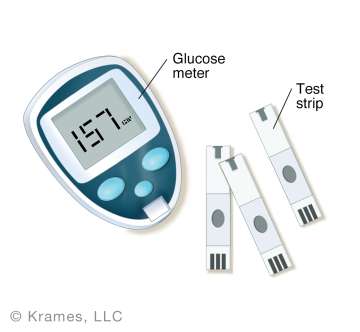
- Test your blood glucose.
- Subtract the blood glucose target from your current pre-meal blood glucose. This result is the number of “points” you wish to lower your blood glucose.
- Divide this result by your correction factor to figure out how much insulin you need for correction.
- Example: Your current blood glucose is 200 mg/dl prior to the meal, and you have a pre-meal target of 100 mg/dl. Your correction factor is 1 unit to lower blood glucose 50 mg/dl (1:50 mg/dl). Therefore, 200 mg/dl (current blood glucose) – 100 (pre-meal target) = 100 mg/dl (“points” to lower or drop glucose). 100 mg/dl ÷ 50 mg/dl = 2 units to correct your blood glucose to target (B).
To Obtain the Total Pre-Meal Insulin Dose (C):
C= A (Insulin dose for carbohydrates) + B (correction dose)
C= 4+2= 6 units
Accurate carbohydrate counting
One of the keys to success when using a basal/bolus insulin regimen is learning how to accurately count carbohydrates. Generally, when you eat carbohydrates you will need to cover them with insulin. Your endocrinologist and diabetes educator will guide you in using various resources to help you accurately count carbohydrates. Usually this information is available on food labels. If food labels are not available, suggested alternative applications include: MyFitnessPal, CalorieKing, Lose-it! and Figwee.
Timing of insulin and accurate dosing
The timing of insulin prior to meals is an important factor in the prevention of high glucose excursions after meals. Rapid-acting insulins, such as Novolog, Humalog and Apidra start working within 10-15 minutes after administration. They peak in about 1-2 hours, and remain active for an average of 4 hours. Regular insulin ideally needs to be injected 30 mins before eating. Newer insulins such as fast-acting insulin Aspart (Fiasp) and Lispro-AABC (Lyumiev) can be injected right before eating.
Since most carbohydrates convert to sugar 30-90 minutes after consumption, it is important to administer the insulin in a timely fashion prior to eating to help prevent high blood glucoses from food.
Self-monitoring of blood glucose
Checking pre- and post-meal blood glucoses will help evaluate the effectiveness of your bolus insulin doses.
-
Adjusting Basal (Long-Acting) Insulin: If your basal insulin dose is correct, your fasting blood glucose should be within target range, and your blood glucose will remain stable (within 30 mg/dl) overnight or throughout the day even if you skip your meal while continuing with your usual physical activity. If your glucose levels are changing by more than 30 mg/dl in a fasted state, review with your provider for recommendations.
- Testing Insulin-to-Carb Ratio: This can be tested when your pre-meal blood glucose is within target range, and you do not need to use correction dosing.
- Take the insulin dose based on your carb ratio to cover the grams of carbohydrates to be eaten.
- Check your blood glucose 2 hours after your first bite.
- To achieve an A1c of 7%, an acceptable 2-hour post meal glucose is less than 180 mg/dl. If you A1c target is different, consult your provider for a specific recommendation.
- Testing Correction Factor:This can be tested when your pre-meal blood glucose is above target range and you don’t plan to eat immediately.
- Give the insulin dose to correct your blood glucose based on your correction factor.
- Check your blood glucose 4-5 hours after taking the correction dose. Your blood glucose should be within 30 mg/dl of target.
- Adjusting Ratios: Ratios are typically adjusted based on identifying a pattern rather than a single blood glucose reading. Ratios are adjusted in consultation with your diabetes team.
- Bedtime Checking: Bedtime checking is always important for multiple reasons. First is to assess the effect of the bolus insulin with dinner. Second is to assess a safe blood glucose level before going to sleep. Third is to evaluate the long-acting insulin dose, especially when compared to your fasting glucose reading.
- Avoid “Stacking” of Insulin: Giving a correction bolus of insulin within 2-hours of the last injection and dropping low is called “stacking.” When a correction dose is given at the peak time of the last bolus, the risk for hypoglycemia increases. It can be very helpful to record the time of your last injected insulin dose to minimize stacking. Various resources such as smart phone apps, glucose logs and special glucose meter devices can help with tracking insulin dosing/timing and reduce stacking. Suggested Applications include D360 or Diabetes 360 and Rapid Calc. Advanced diabetes technology products like smart pens and insulin pumps can also help reduce the risk of stacking. Consult with your diabetes team to discuss options.
Record keeping
Your diabetes team may ask you to log or record your food intake and insulin dosing to evaluate your insulin-to-carbohydrate ratio and ensure dosing is accurate.
Key Information to Log:
- All food and beverages consumed
- Quantity of each food item
- Grams of carbohydrates
- Dose, type and timing of insulin
- Physical activity
Suggested Apps: MySugr, Glucose Buddy, MyNetDiary
Suggested Apps for various Continuous Glucose Monitor (CGM) device users:
-Dexcom: undermyfork, Sugarmate and Dexcom event marker and in conjunction with InPen app
-Libre: Libre app event marker and notes section
-Medtronic: Guardian Connect, or in conjunction with InPen app
Insulin injection technique videos
- Step-by-Step: vial and syringe
- Step by step: insulin pen video
- Step by step: how to mix two types of insulin by syringe


Injecting Insulin - site selection
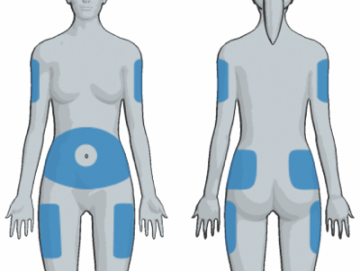
Site selection: Insulin must be injected in subcutaneous tissue (fat tissue just under the skin) for optimal absorption. Do not inject insulin in muscle. The best location for injecting insulin is the abdomen (further than 2 inches away from the navel). Other areas that can be used include the upper buttocks, the back of the upper arms (where the most fat is located) and the upper outer thighs – but absorption may be more unpredictable in locations outside the abdomen. Please note, the absorption can vary in different parts of the body depending on the amount of fat tissue and activities engaged in following an injection. Consult your diabetes team for more specifics on what injections sites work best for you.
Site inspection: It is important to rotate injection sites. Injecting in the same place too often can cause scar tissue, hard lumps or extra fat deposits to develop. These areas can change the way insulin is absorbed, making it more difficult to keep your blood glucose on target. Always inspect your sites and feel for lumps and hard spots – avoid injecting in those sites for at least 3 months.
Site rotation: Always inject at least one inch away from a recent injection site. Rotate your sites often for best absorption.
General Insulin Storage Guidelines
Store unopened, not-in-use insulin in the refrigerator. These are good until the stamped expiration date on the box or product. Never freeze or expose insulin to direct heat or sun.
Store opened, in-use insulin at room temperature. Discard as instructed even if there is insulin left in the vial or pen. Never freeze or expose to direct heat or sun. The following are recommendations from manufacturers for length of use of vials and pens once opened or taken out of refrigerator:
Vials
- Lantus, Novolog, Humalog, Admelog, Apidra: Discard vial 28 days after opening.
- Levemir: Discard vial 42 days after opening.
- Novolin (R, N, 70/30): Discard vial 42 days after opening.
- Humulin (R, N, 70/30): Discard vial 28 days after opening.
- Novolog Mix 70/30, Humalog Mix 75/25: Discard vial 28 days after opening.
Pens
- Lantus, Novolog, Humalog, Admelog, Apidra: Discard pen 28 days after opening.
- Toujeo: Discard pen 56 days after opening.
- Tresiba: Discard pen 8 weeks after opening.
- Levemir: Discard pen 42 days after opening.
- Humulin N: Discard pen 31 days after opening.
- Humulin 70/30: Discard pen 31 days after opening.
- Novolog Mix 70/30: Discard pen 14 days after opening.
- Humalog Mix 75/25: Discard pen 10 days after opening.
Disposing of Syringes and Needles

After you inject, put the needle or syringe directly in a sharps container. Never lay them down anywhere and don’t recap the needle.
When the sharps container is full, put it into a garbage bag and secure the top. Label the bag “needles” or “sharps". Call your local waste company to ask about disposal requirements for needles.
Helpful resources
