Reflux After Sleeve Gastrectomy
Find your care
Our bariatric surgeons use a range of treatments to help you reach weight loss goals and optimize your health. To learn more, call 310-206-0367.
Heartburn is an uncomfortable sensation or pain in your chest, just behind the sternum, or breastbone. It is caused by the acid secreted in stomach travelling up in the esophagus (acid reflux). If the symptoms of acid reflux happened more than twice a week, you might have a condition called gastroesophageal reflux disease (GERD). Acid reflux after sleeve gastrectomy is a frequently discussed topic among bariatric surgeons.
Many studies have shown that approximately 30% of gastric sleeve patients may experience new reflux among patients who never had acid reflux before surgery. On the other hand, among the patients who have mild to moderate symptoms of reflux before sleeve gastrectomy, most patients feel symptomatic relief after surgery because the weight loss can decrease the intra-abdominal pressure. A subset of patients with reflux prior to surgery may experience worsening of acid reflux after surgery.
What is the cause of reflux after sleeve gastrectomy?
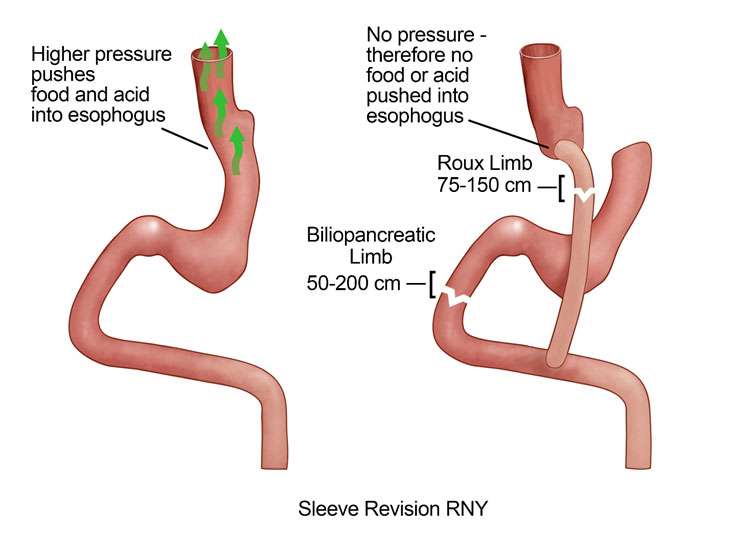
After sleeve gastrectomy, the stomach is significantly smaller and can only hold 100-300 ml of food/liquids at one time. Therefore, the pressure within the smaller stomach is significantly higher. The Lower Esophageal Sphincter (LES) usually can prevent the stomach content to travel into esophagus. However, with much higher pressure after sleeve gastrectomy, some gastric content/gastric acid get pushed into the esophagus, causing reflux.
What are the treatment options for acid reflux after sleeve gastrectomy?
If you have developed reflux symptoms after sleeve gastrectomy, lifestyle modification and dietary changes are the first line treatment. Small and frequent meals may reduce the amount of food in the stomach and thus reduce the pressure and reflux. Try to avoid eating too much at one time and eating late at nighttime.
If lifestyle modification and dietary changes fail to alleviate reflux symptoms, a number of over-the-counter and prescription medications are the next choice. Histamine antagonists (H2 blockers) and proton pump inhibitors (PPIs) are the two types of acid reducers that can lead to long time symptomatic relief. Famotidine (Pepcid AC) and Cimetidine (Tagamet HB) are two common OTC H2 blockers. Commonly used OTC PPIs include esomeprazole (Nexium 24HR), lansoprazole (Prevacid 24HR), and omeprazole (Prilosec OTC). PPIs are more potent in reducing acid secretion than H2 blockers. They are the preferred medications for severe heartburn. If the OTC dose of PPI fails to control the heartburn symptoms, higher dose of PPIs should be considered and prescribed by the physicians.
For sleeve gastrectomy patients with severe reflux/heartburn despite using the higher dose of PPIs, conversion to Roux-en-Y gastric bypass surgery should be considered. Unlike the high pressure system in the remaining stomach after sleeve gastrectomy, the pressure in the stomach pouch after Roux-en-Y gastric bypass surgery is low. There is no pressure to push the food/acid up into the esophagus after gastric bypass surgery, thus significantly reducing the acid exposure. Long-term follow-up data suggested that more than 90% of patients could achieve resolution of GERD symptoms after the revision surgery.
For sleeve gastrectomy patients with mild/moderate reflux symptoms who have regained significant amount of weight, conversion to Roux-en-Y gastric bypass surgery may lead to both weight loss and resolution of reflux symptoms. For those patients who had difficulty eating due to the severe reflux, the weight loss after conversion to Roux-en-Y gastric bypass surgery might be very limited. However, most patients reported dramatically improved quality of life because they do not have heartburn anymore.
Contact Us
To schedule a consultation with UCLA Bariatric Surgery in Los Angeles, California, call us at 310.206.0367 or fill out our online form
For a physician referral, please call (800) UCLA-MD1 (825-2631).
*Weight loss results can vary depending on the individual. There is no guarantee of specific results. Read full disclaimer.