Clinical Updates
Abdominal | Breast Imaging | Cross Sectional Interventional Radiology | Diagnostic Cardiovascular Imaging | Diagnostic Neuroradiology | Interventional Neuroradiology | Interventional Radiology | Musculoskeletal Imaging | Pediatric Imaging | Thoracic Imaging
Abdominal Imaging
MR-targeted Biopsy Poised to Become the New Standard in Prostate Cancer Diagnosis
Research advances at UCLA with funding from the National Cancer Institute have led to major changes in the way prostate cancer is diagnosed and managed. Targeted MR-guided biopsy via either magnetic resonance-ultrasound (MR-US) fusion or direct MR-guided biopsy is emerging as the best way to detect, grade and stage prostate cancer. Prostate cancer care has been challenging in part because of the difficulty in distinguishing patients with non-aggressive cancer who do not need treatment from those with aggressive disease who do.
A Wide Range of Treatment Options Helps Provide Optimal Care for Women with Uterine Fibroids
More than half of all women develop fibroids — benign growths in the uterine wall — by age 50. The cause is not clear, though heredity seems to play a role. Most women with uterine fibroids are asymptomatic or experience only minimal discomfort. But up to one-fourth may experience excessive menstrual bleeding, frequent urination, pain or pressure in the pelvis and back, an enlarged abdomen, painful intercourse and infertility.
Typically discovered on routine pelvic exam and pelvic ultrasound, fibroid size, type, location and number are best confirmed by magnetic resonance imaging (MRI).
UCLA's unique, multidisciplinary program was the first in the country to offer minimally invasive, non-invasive and robotic surgical treatments for uterine fibroids and adenomyosis.
MRI-ultrasound Fusion Permits Targeted Biopsy for Prostate Cancer
A team of UCLA experts has introduced refinements to targeted biopsy of prostate cancer, greatly improving the ability to distinguish men who should have treatment from those who could defer. The new targeted biopsy protocol, developed by UCLA radiologists, urologists, pathologists and biomedical engineers, can permit active surveillance with a confidence not previously available. Aggressive treatment, like surgery or radiation therapy, may not be necessary for many of the 230,000 men diagnosed each year with prostate cancer. On the other hand, targeted prostate biopsy can, more efficiently than conventional biopsy, identify men who should be treated — such as those with potentially lethal cancers — allowing prompt and appropriate intervention.
Ultrasound/MRI Biopsy Enhance Treatment for Prostate Tumors
Unlike most other cancers, prostate tumors are often not lethal and may never require treatment. With active surveillance, patients who have non-aggressive tumors can be spared the pain, risks and side effects of surgery or radiation therapy. The problem has been finding reliable ways of predicting which patients need treatment and which ones can simply be monitored. A UCLA team of urologists, radiologists, pathologists and biomedical engineers is now advancing a new approach that could dramatically improve the prostate biopsy and thus lead to better-informed treatment decisions.
Advanced Imaging Techniques Improve Prostate Cancer Care
About half of the men diagnosed with prostate cancer have low-risk tumors that make them good candidates for active surveillance: regular monitoring of prostate-specific antigen (PSA); annual biopsies; and a Gleason score, which grades cancer cells by how they look compared to normal cells. Active surveillance allows men with small, confined and nonaggressive tumors to avoid surgery or radiation treatments that expose them to the risk of incontinence and erectile dysfunction. However, in three out of 10 cases, standard active surveillance techniques fail to identify the aggressiveness of prostate tumors.
High-Tech Imaging Improves Surgical Outcomes for Prostate Cancer
State-of-the-art magnetic resonance imaging (MRI) technology at UCLA is driving key advances in the diagnosis and treatment of prostate cancer. MRI assists surgeons both prior to and during robotic-assisted prostatectomy and by potentially enabling more minimally invasive treatment.
New Treatment Available for Uterine Fibroids
An estimated 50 to 70 percent of women have uterine fibroids noncancerous growths that tend to develop during childbearing years. Most women are unaware that they have them, but 20 to 40 percent of women older than 35 experience symptoms, most commonly heavy menstrual flow.
Newer Imaging Techniques Superior in Detecting and Localizing Prostate Cancer
Magnetic resonance (MR) imaging is playing an increasingly important role in the case of prostate cancer patients, including prostate cancer detection, disease staging and treatment planning. At UCLA, a team of radiologists, urologists, MRI scientists and technologists work together using advanced prostate imaging and surgical techniques, including robotically assisted prostatectomy, to enable more precise diagnosis and treatment. UCLA is also planning studies using MR imaging to guide highly accurate, non-invasive treatments for prostate cancer.
Virtual Colonoscopy Offers Visualization of Colon in Less Invasive Procedure
Virtual colonoscopy, also known as 'CT colonography' because the images are created by three-dimensional reconstruction of high-resolution CT (computed tomography) images, offers visualization of the colon similar to that of an optical colonoscopy in a less invasive and less time-consuming procedure.
Breast Imaging
Tissue Density May Influence Risk for Breast Cancer
The breast is composed of fat and glandular tissue - the higher the proportion of glandular tissue, the denser the breast. It is more difficult for a radiologist to spot a potential tumor in dense breast tissue, which means cancer may be missed during mammography. Independent of detection challenges, studies also show that women with dense breast tissue have a higher risk of developing breast cancer, says Lawrence Bassett, MD, a professor of radiology and section chief at the Iris Cantor Center for Breast Imaging.
"Most experts now believe that there is a risk factor involved in breast density," he says. "It makes some sense because breast tumors don't come from fat; they come from broglandular tissue."
However, there are no guidelines from medical organizations on whether or not women with dense breasts who are at average risk for breast cancer should undergo additional screening or have a different type of screening, such as a digital breast tomosynthesis (3-D mammography), MRI or ultrasound. "We know additional imaging will pick up more breast cancer, but we don't have long-term data to suggest that will actually help with survival rates," Dr. Bassett says.
Advanced 3D Mammography Leads to More Accurate Breast Cancer Detection
Digital breast tomosynthesis is emerging as the new gold standard in mammography. Also known as 3D mammography, this breast imaging technology provides radiologists with multiple, thin-section images through the breast, increasing breast-cancer detection rates while reducing the rate of false-positive results.
Digital Breast Tomosynthesis Marks a New Era in Breast Imaging
UCLA is among the first medical centers in the region — and the only one in West Los Angeles — to offer a new breast imaging technology that improves breast cancer detection rates compared to conventional mammography while reducing the rate of false-positive results. Called digital breast tomosynthesis, the technology is now offered at two UCLA breast imaging centers and is expected to emerge as the new standard-of-care in breast imaging.
UCLA Breast Center at Santa Monica
Launched in June 2012, the UCLA Breast Center at Santa Monica is one of only a handful in the nation that employ a patient navigator who gathers medical reports, coordinates appointments, answers questions and serves as the patient’s single point of contact for the healthcare team.
New Santa Monica-UCLA Women's Imaging Center
The newly opened Santa Monica-UCLA Women's Imaging Center features the latest imaging technology within a comfortable, private setting dedicated exclusively to women during regular business hours. The 5,200-square-foot facility, which joins the Iris Cantor Center for Breast Imaging in Westwood as part of the UCLA Women's Imaging network, is located at 1260 15th St., Suite 111, near the Santa Monica-UCLA Medical Center and Orthopaedic Hospital campus. In addition to all-digital mammography, both centers perform breast ultrasound studies, image-guided diagnostic biopsies, breast MRI studies and cardiac imaging in a private and serene environment. They are staffed by radiologists who specialize in breast imaging, mammography technologists, ultrasound technologists, and by support staff.
Women's Imaging Services Brochure
The newly opened Santa Monica-UCLA Women's Imaging Center features state-of-the-art imaging technology in a convenient and comfortable setting designed exclusively for women during regular business hours. Throughout their treatment, women are cared for in a relaxing, spa-like setting warm, soothing and private.
Recent Study Shows Benefits of Digital Mammography for Many Women
A landmark study, in which UCLA participated, has shown that digital mammograms are 15 to 28 percent more effective than standard film mammograms in detecting tumors in women with dense breast tissue, those who are pre- or perimenopausal (women who had their last menopausal period within 12 months of their mammograms), and those younger than 50 years of age.
Cross Sectional Interventional Radiology
MR-guided Ultrasound and Robotic Surgery Expand Options for Women with Abnormal Uterine Bleeding
UCLA is the only center in California to offer magnetic resonance guided focused ultrasound surgery (MRgFUS), an innovative, non-invasive procedure combining magnetic resonance imaging (MRI) and ultrasound technologies to precisely target and destroy uterine fibroids without incisions, needles or catheters.
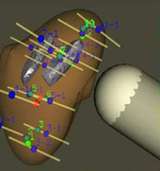
Percutaneous Ablation May be the Best Treatment Option for Many Small Liver Tumors
Surgical resection, usually the first local treatment option considered for patients with liver tumors, may not be suitable for all patients. Percutaneous ablation now offers the best option in treating most small tumors, such as primary hepatocellular carcinoma. Further, percutaneous ablation offers a local treatment option to supplement systemic therapy, in those with liver metastases who might benefit from this treatment. With this minimally invasive procedure, patients usually go home the same day or after an overnight hospital stay, usually with only minor side effects if any. Major complications occur in only up to 3 percent of cases.
Diagnostic Cardiovascular Imaging
UCLA is the First Center in the Western United States to Offer Routine MRI for Pacemaker Patients
With a level of detail and clarity not offered by other imaging tools, magnetic resonance imaging (MRI) often provides critical diagnostic information that isn’t available using imaging techniques such as computed tomography (CT) or ultrasound. Moreover, as the American population ages, the number of MRI scans performed each year increases — as does the number of people with implanted cardiac devices.
MRI Helps Diagnose and Treat Common Heart Defect
Hypertrophic cardiomyopathy is an inherited heart defect that is a common cause of sudden cardiac death in young people. The condition, which affects an estimated one in 500 people, causes the muscle mass of the left ventricle to thicken abnormally, forcing the heart to work harder to pump blood. Some patients are diagnosed after developing persistent symptoms, which include shortness of breath, dizziness, fainting and chest pain. Other patients may experience no symptoms and live a normal life with no heart-related problems, or they may unsuspectingly develop fibrosis (scar tissue) that eventually causes life-threatening cardiac arrhythmias (abnormal heart rhythms) or even sudden cardiac death. But by using magnetic resonance imaging (MRI), physicians are now able to get a better look at scar tissue in the heart muscle, making it easier to decide when and how to intervene in affected patients.
Online, Remote Control Cardiovascular Imaging Technology Boosts Efficiency, Allows Access to Distant Expertise
New remote imaging technology available at UCLA offers patients and referring physicians greater access and improved scheduling flexibility for diagnostic cardiovascular imaging services. UCLA radiologists and Siemens Medical Solutions have jointly developed software that enables imaging experts at UCLA hospitals in Westwood and Santa Monica to use a computer via a secure Internet connection to operate a magnetic resonance imaging (MRI) machine at a remote location to conduct these high-demand imaging studies.
Speedy Dual-source CT Scanners Improve Safety, Effectiveness of Diagnostic Cardiovascular Testing

UCLA now uses the fastest computed tomography (CT) scanners available for cardiovascular imaging, significantly enhancing the safety and capabilities of this noninvasive diagnostic tool. The dual-source computed tomography (DSCT) technology slashes the time required for data acquisition in half by using two X-ray tubes and two 64-row detector arrays double the number found in traditional systems.
How and Why CT Scanners are Evolving
The advent of dual-source CT scanners represents a significant step up in the evolution of CT machines. Designed with two X-ray tubes and two detector arrays, the dual-source scanner captures data nearly twice as fast as previous scanners. "The dual-source CT scanner is ideal for cardiac imaging," says Stefan Ruehm, M.D., Ph.D., associate professor of radiology at UCLA Medical Center. "It's a rather noninvasive diagnostic tool that allows a physician, with a very high negative predictive value, to determine whether or not the patient has coronary artery disease," he says.
How New CT Scanners are Improving Cardiac Care
Innovation is a powerful tool, especially in the field of medicine, where it can save lives. The latest advancement, a new generation of noninvasive scanners, allow physicians the capability to provide early-stage cardiovascular diagnostics. The goal is to detect potential heart problems early, before any damage is done. "Traditionally, the workup for heart disease started with the onset of chest pain and the whole target was the managing of clinical heart disease," says Jonathan Goldin, M.D., Ph.D., associate professor of cardiothoracic radiology at UCLA Medical Center. "Now the target is identifying early vascular disease way before symptoms develop."
Fast CT Scan Helps Detect Heart Disease
Early detection of heart disease can save lives. "When symptoms of heart disease occur, significant blockage of the coronary artery already exists," notes Jonathan Goldin, M.D., Ph.D., associate professor of cardiothoracic radiology. New noninvasive imaging technologies are allowing physicians to more easily and accurately obtain images of the heart that can reveal both early disease and critical artery narrowing or blockages.
Care for coronary artery disease is currently moving to a more aggressive model, emphasizing prevention and targeting people who are at risk for developing the condition in order to make the diagnosis early. The traditional model has been to wait for symptoms to present and then try to find their cause; but with coronary artery disease, by the time symptoms appear, a significant blockage of the artery exists so that the blood supply to the heart is compromised or completely cut off. Traditional diagnosis using angiogram presents too great a risk for patients who are asymptomatic or who have only subtle symptoms. The changing approach to aggressively diagnose early calls for less invasive diagnostic tests.
Diagnostic Neuroradiology
Using Heat to Kill Spinal Tumors Can Improve Quality of Life for Patients with Bone Metastasis
A procedure called radiofrequency ablation (RFA) is a reliable tool for the treatment of various pain conditions, as well as the destruction of some types of so -tissue tumors when conventional surgery is not an option. RFA also has emerged as a successful approach to alleviating the intense pain experienced by cancer patients with bone metastases.
Radiofrequency Ablation for Pain Palliation in Patients with Spinal Metastases
Radiofrequency ablation (RFA) is a reliable tool for the treatment of various pain conditions as well as the destruction of some types of soft-tissue tumors, such as liver or lung lesions, when conventional surgery is not an option. In recent years, however, RFA has emerged as a highly successful approach to alleviating the intense pain experienced by cancer patients with bone metastases. UCLA is one of only a few centers in the country with experts trained to offer RFA for this type of palliative care and is working with oncologists throughout the region to identify patients who may benefit.
New Brain Imaging Technique Helps Predict Patients Response to Avastin
Glioblastoma is the most common and deadly type of primary brain tumor in adults. On average, glioblastoma patients survive only 12 to 15 months after initial diagnosis despite conventional treatment with surgery, chemotherapy and radiation. The prognosis for patients with recurrent glioblastoma is worse. Food and Drug Administration (FDA) approval of the drug Avastin represented the first new systemic therapy shown to be effective against recurrent glioblastoma in more than 10 years, but the majority of patients with recurring brain tumors do not respond to the drug.
Non-invasive Testing, Earlier Surgery can Stop Seizures in Tuberous Sclerosis Complex
Anya, now two-and-a-half years old, underwent the surgery at UCLA when she was 16 months old. After suffering up to 30 seizures a day and her medications not working as effectively, Dr. Wu and her team suggested that Anya be evaluated for surgery to remove the offending tubers. She then underwent the non-invasive testing and was found to be a good candidate for surgery. It has been more than a year since her seven-hour operation, and she is still seizure-free. UCLA's non-invasive approach uses a combination of magnetic resonance imaging (MRI), fluoro-deoxyglucose positron emission tomography (FDG-PET) and magnetic source imaging (MSI) to identify the area of brain to be removed.
PET/CT Technology Used to Diagnose Cancer and Dementia
PET-CT imaging technology allows specialists to provide diagnostic services for the evaluation of cancer and dementia at Santa Monica-UCLA Medical Center and Orthopaedic Hospital (SM-UCLA&OH). The procedure can provide staging information in cancer patients, or can be conducted to evaluate dementia or therapy-refractory seizure disorder.
Interventional Neuroradiology
Stroke Care Improves, but Patients Need to Act FAST
Stroke symptoms can include weakness or numbness on one side of the body, vertigo, nausea, difficulty understanding or speaking and impaired coordination. In the face of a possible stroke, remember the acronym FAST: Face drooping, Arm weakness, Speech difficulty and Time to call 911.
Hospital on Wheels Brings Immediate Care to Stroke Patients
UCLA Health has launched the first mobile stroke unit on the West Coast, enabling rapid delivery of brain-saving medications to stroke patients who might otherwise face debilitating delays in treatment. The unit consists of an ambulance equipped with CT scanning technology along with highly trained personnel who respond to calls involving patients suspected of having a stroke. The team is able to perform diagnostic testing and initiate appropriate treatment before transporting the patient to the hospital for further care.
Flow Diversion Stents Provide Treatment Option for Unruptured Cerebral Aneurysms
About 35,000 Americans suffer potentially life-threatening cerebral aneurysm ruptures each year. A much larger number of people develop unruptured aneurysms — areas of weakness within a major blood vessel in the brain that bulge and are at risk of rupture and hemorrhage. Unruptured aneurysms can remain asymptomatic and undiagnosed. In some cases, the problem is discovered incidentally, when a patient undergoes imaging for generalized neurological complaints, such as headache or dizziness.
When 'Time is Brain,' Prompt Response Essential to Successful Stroke Treatment
As the first point of contact in quickly assessing and intervening with patients brought to the UCLA Comprehensive Stroke Center, the interventional neuroradiology team plays a key role in the success of UCLA’s stroke program.
When patients in Los Angeles appear to be suffering from acute stroke, emergency responders use the Los Angeles Prehospital Stroke Screen, a tool validated at UCLA, to identify those who should be transferred to the UCLA Comprehensive Stroke Center for potential interventional treatment. For patients who are routed to UCLA, the “brain attack” team is activated. After an initial rapid evaluation to determine whether the patient is suffering from an acute stroke as opposed to a stroke mimic, the team ensures that the patient is stable before further assessment using advanced imaging — either CT or MRI. If stroke intervention is indicated, the front-line treatment is medical, in the form of intravenous tissue plasminogen activator (tPA), a clot-busting drug that can be administered effectively up to four-and-a-half hours after an acute stroke.

Pivotal Clinical Trial Investigates Flow Diversion Device for Brain Aneurysm
UCLA’s Division of Interventional Neuroradiology is participating in a multi-center U.S. clinical trial to evaluate the safety and efficacy of the MicroVention, Inc. Flow Re-Direction Endoluminal Device Stent System (FRED™) for the treatment of intracranial aneurysms.
The prospective study aims to answer key questions on use of the FRED stenting system for wide-necked or large intracranial aneurysms. While treatment of these types of aneurysms has been particularly vexing, the new stenting system holds the promise of improved clinical outcomes and fewer procedure-related complications.

Specialists Use Surgical and Endovascular Techniques to Improve Care for Cerebrovascular Patients
In the past, cerebrovascular conditions such as stroke and cerebral aneurysms were treated almost exclusively with surgical techniques that required a craniotomy. Today’s latest neurovascular techniques, however, chart smarter, and less risky, pathways to treat problems in hard-to-reach areas of the brain.
Blood-clot Retriever Developed at UCLA Outperforms Previous-generation Device to Gain FDA Approval
A device being tested for removing blood clots from the brains of stroke victims proved so superior to existing technology that the clinical trial was stopped early and the new device was approved in March 2012 by the Food and Drug Administration (FDA) for use in patients. The Solitaire Flow Restoration Revascularization Device, which was developed and tested at UCLA, is a next-generation blood-clot retriever that can restore blood flow in stroke victims and preserve brain cells.

New Device to Treat Stroke Patients is "Game-Changer"
By using SOLITAIRE in combination with tPA, physicians at advanced stroke centers will be able to reliably open the arteries in 80-90 percent of their patients, an unprecedented success rate. A newly approved device to remove blood clots from blocked brain arteries in people experiencing a stroke heralds a new era in the treatment of the fourth-leading cause of death and No. 1 cause of long-term disability in the United States.
Glue Procedure for Hard-to-Treat Brain Aneurysms
UCLA offers a new "glue procedure" to treat brain aneurysms that cannot be repaired by conventional methods. A liquid glue-like substance that functions as an embolic agent is injected into an artery's abnormal bulge (aneurysm) using a small tube threaded up an artery in the groin. The polymer fills up the aneurysm, preventing additional blood from entering, and thereby eliminating the risk of rupture. Securing an aneurysm is crucial: 50 percent of patients with a burst aneurysm die instantly.
Brain Aneurysm and AVM Program: Program Update
The UCLA Brain Aneurysm and AVM Program is a world leader in the diagnosis, treatment and management of vascular diseases of the brain and spinal cord. These diseases include aneurysm, arteriovenous malformation (AVM), cavernous angioma, stroke and carotid and intracerebral stenosis. UCLA benefits from the skill and experience of a multidisciplinary team of experts who work collaboratively to understand the complete physiopathology of each patients disease and carry out an optimal treatment plan.
New Treatment can Improve Chances of Survival
The UCLA Medical Center lays claim to pioneering the way that brain aneurysms are treated. Developed by a former faculty member about 15 years ago, the Guglielmi Detachable Coil (GDC coil) is now a standard alternative or supplement to neurosurgery for treating brain aneurysms. "Coils have dramatically altered the landscape for treating aneurysms," says Dr. Gary Duckwiler, professor of interventional neuroradiology at UCLA Medical Center. "In the United States, we now have about 50 percent of the aneurysms being treated by coiling, whereas this treatment didn't even exist before 1990."
New Study Shows Superior Outcomes for Treating Ruptured Aneurysms with Endovascular Coil
Cerebral aneurysms can result in subarachnoid hemorrhages bleeding in the space filled with cerebrospinal fluid that surrounds the brain. The consequences of such hemorrhages can be devastating, with 70 percent of patients either dying or suffering severe, disabling stroke. The recent International Subarachnoid Aneurysm Trial (ISAT) compared the outcomes of patients treated for a ruptured intracranial aneurysm with the standard surgical technique open craniotomy and surgical clipping and those treated with a detachable endovascular coil. Overall, patients treated with an endovascular coil experienced better outcomes than those treated with conventional surgery. The ISAT patients treated with an endovascular coil were found to have a 7.4 percent lower risk of death or dependence than those who underwent craniotomy and clipping.
Interventional Radiology
UCLA is among the first medical centers to offer a minimally invasive alternative to knee replacement surgery, providing potential relief to individuals who are experiencing debilitating pain from knee arthritis but haven’t been candidates for surgery or were deterred by the lengthy recovery time.
UCLA Specializes in Inferior Vena Cava Filter Placement and Removal
For decades, inferior vena cava (IVC) filters have been recommended for select patients to prevent blood clots from traveling to the heart and lungs. While they are very successful at preventing pulmonary emboli (PE), the devices are now at the center of significant controversy. The U.S. Food and Drug Administration has received hundreds of adverse-event reports relating to IVC filter migration, perforation and fracture, and the devices have been the subject of a number of lawsuits. The FDA recommends the removal of IVC filters as soon as protection from blood clots is no longer needed.
Aortic Disorders Require Prompt Diagnosis and Treatment
Accurate diagnosis and prompt treatment of abnormalities of the aorta are vital to achieving good patient outcomes. Unfortunately, many disorders of this arterial trunk that carries oxygen-rich blood from the heart to the branch arteries are “silent,” failing to present symptoms until the damage is advanced.
UCLA is first center in California to offer minimally invasive procedure for removing blood clots
UCLA is the first medical center in California to offer a minimally invasive procedure to remove blood clots from patients with deep vein thrombosis and/or pulmonary embolism. The new procedure uses an FDA-approved device called the AngioVac, which vacuums the blood clot out of the vein and filters out solids before returning the cleansed blood to the patient. An alternative to surgery, the procedure is available to many patients with blood clots in the lungs or blood vessels deep in the body, especially the pelvis or belly, that are at risk of breaking off and traveling to the heart or lungs.
3-D Imaging Techniques Transform Cardiac Catheterization
The field of cardiac catheterization has benefited significantly from the advent of two technologies that create 3-D images. The techniques — rotational angiography and the fusion of X-ray and MRI/CTA — are changing the way catheterizations are performed on patients with cardiovascular disease. These state-of-the-art imaging techniques facilitate catheter-based minimally invasive interventions on patients who previously would have required surgery, thus decreasing the hospital stay, time in intensive care, recovery time and the amount of pain suffered.
From Surgery to Interventional Radiology to Cardiology, Treatment Options for Vascular Disease Expand
Treatment options for vascular disease have expanded significantly in the last two decades. UCLA now offers a host of state-of-the-art therapies delivered by vascular surgeons, interventional radiologists and cardiologists, including endovascular repair for aneurysms and ischemic vascular disease.
Uterine Fibroid Embolization Provides a Less Invasive Alternative to Hysterectomy
UCLA offers uterine fibroid embolization (UFE) for the treatment of uterine fibroids, which are non-cancerous tumors estimated to affect as many as 77 percent of American women. The presence of fibroids, generally diagnosed during a gynecologic internal exam, is most frequently confirmed by an abdominal ultrasound. Magnetic resonance or computer tomography imaging techniques may also be used to confirm diagnosis.
New Treatments for Osteoporosis
Known as a silent disease, osteoporosis gradually thins and weakens bones, often without people being aware they have it. If not detected early, the first symptoms of osteoporosis can be a broken bone or fracture. Men as well as women are susceptible to this disease. The good news is that osteoporosis can be treated. When diagnosed early through screening tests, minimally invasive treatments are available that achieve fracture stabilization. "We are now doing procedures such as kyphoplasty earlier and earlier so that patients don't have to suffer the consequences of prolonged pain," says Cheryl Hoffman, M.D., director of interventional radiology at the UCLA-Santa Monica Medical Center.
Musculoskeletal Imaging
FDG-PET/CT Imaging can Help Guide Treatment Strategies for Patients with Soft Tissue Sarcomas
To ensure patients with soft tissue sarcoma receive the most effective therapy possible, UCLA clinicians use FDG-PET/CT scans (positron emission tomography/computed tomography using radio-labeled [18F]-fluorodeoxyglucose) to identify the most effective treatment strategies and to direct patient care.
Improvements to Imaging Technology Benefit Ortho Patients
State-of-the-art imaging technology has expanded options for orthopaedic patients while providing a clearer picture of their condition. "Imaging is the cornerstone for confirming diagnoses that we suspect on physical findings," says Leanne Seeger, M.D., chief of musculoskeletal imaging in the UCLA Department of Radiology. "Obviously, patients want to know what's wrong with them, and with the tools we now have we are able to be much more definitive in what we can tell them."
Ultrasound, MR Arthrography Enhance Musculoskeletal Imaging Tools
In addition to the latest radiographic, magnetic resonance imaging (MRI) and computed tomography (CT) equipment, UCLA radiologists and technologists use ultrasound and MR arthrography imaging techniques to enhance diagnostic capabilities for certain musculoskeletal injuries and disorders. These tools offer orthopaedic and rheumatology patients the complete array of diagnostic modalities.
UCLA Radiology can provide your practice with an imaging package for dental implant patients that offers paraxial and panoramic views produced by our new high-speed 64-slice Multi-Detector Computed Tomography (CT) system to assist in pre- and post-implant planning. This procedure also is available on our Sensation 16 system. The imaging study is performed under the direction of Dr. Kambiz Motamedi, musculoskeletal radiologist.
Pediatric Imaging

Protocols for Pediatric Radiology: Children Are Not Small Adults
Imaging technologies like ultrasonography (US), computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) have improved the ability of pediatric radiologists to diagnose complex cases in children.
Is CT Imaging Safe for My Child?
New imaging protocols for computed tomography (CT) scans have been adopted at all UCLA facilities to help reduce the risk of radiation exposure to children undergoing this very beneficial, often life-saving, procedure. A CT scan is a medical imaging method that uses X-rays to generate detailed, specialized images of a body structure. According to M. Ines Boechat, M.D., F.A.C.R., chief of Pediatric Imaging at UCLA Mattel Children's Hospital and current president of the Society for Pediatric Radiology, it is often the gold standard for diagnosing many illnesses and injuries. "CT scans produce images of excellent quality with a very short time of radiation exposure," she explains.
Thoracic Imaging
New Protocol Improves Diagnosis of Thyroid Nodules
Thyroid cancer is the fastest-rising malignancy in the United States, with rates tripling since the 1970s. Thyroid nodules are also common. About half of adults develop one or more nodules by age 40. Most nodules are benign, but require diagnostic tests for assessment. Four percent of nodules are malignant.
Advanced Imaging Techniques Aid Cancer Diagnosis, Treatment
As researchers and clinicians continue to expand the limits of what can be done to effectively diagnose and treat cancer, the role of experts in radiological sciences is increasing. "People who are diagnosed with cancer are living much longer, and it is now more important than ever that we provide a fully integrated, multidisciplinary approach to manage the disease from diagnosis to staging to therapy to therapy-response monitoring," says Jonathan Goldin, M.D., Ph.D., chief of radiology at Santa Monica-UCLA Medical Center and Orthopaedic Hospital and vice clinical chair in the UCLA Department of Radiology.
UCLA Lung Screening Clinic Monitors High-risk Patients to Catch Lung Cancer Early
The UCLA Lung Screening Clinic offers a sophisticated program to monitor high-risk patients with high-quality computed tomography (CT) imaging while exposing them to substantially less radiation than a typical CT scan. The clinic is a collaborative effort that brings together UCLA experts in thoracic imaging, pulmonary medicine, medical oncology, radiation oncology and thoracic surgery in a program designed to monitor at regular intervals patients at high risk for developing lung cancer.