Vascular Access Procedures
Find your care
Our board-certified physicians diagnose and treat many vascular conditions. Call 310-481-7545 to learn more about interventional radiology services.
Permacath
Treatment for:
Venous access
Why it’s done:
Permacaths provide long-term central venous access for treatments which require high flow rates, such as dialysis or plasmapheresis.
How it’s done:
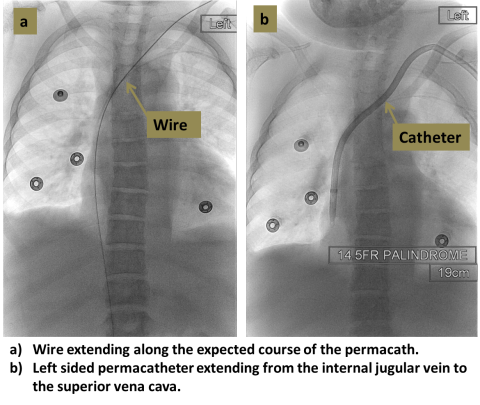
An interventional radiologist uses ultrasound to access the target vein, most commonly the internal jugular vein in the neck. X-rays are then used to guide placement of the catheter so that the tip lies in the central veins near the heart. The catheter is tunneled beneath the skin and exits the skin usually in the upper chest.
Level of anesthesia:
Conscious sedation
Risks:
Small risk of bleeding or infection. Catheters can sometimes break or clog, necessitating replacement. X-rays are used.
Post-procedure:
One to three hours in recovery, then discharge home. The catheter can be used immediately. The catheter exit site should be kept clean and dry.
Follow-up:
With referring physician. If problems with the catheter occur, contact your interventional radiologist.
Hickman or Groshong catheter placement
Treatment for:
Venous access
Why it’s done:
Hickman or Groshong catheters provide long-term central venous access for treatments such as chemotherapy, TPN, or antibiotics, and can be used for blood draws. A Groshong catheter has a valve at the tip, while Hickman catheters do not.
How it’s done:
An interventional radiologist uses ultrasound to access the target vein, most commonly the internal jugular vein in the neck. X-rays are then used to guide placement of the catheter so that the tip lies in the central veins near the heart. The catheter is tunneled beneath the skin and exits the skin usually in the upper chest.
Level of anesthesia:
Conscious sedation
Risks:
Small risk of bleeding or infection. Catheters can sometimes break or clog, necessitating replacement. X-rays are used.
Post-procedure:
One to three hours in recovery, then discharge home. The catheter can be used immediately. The catheter exit site should be kept clean and dry.
Follow-up:
With referring physician. If problems with the catheter occur, contact your interventional radiologist.
Peripherally inserted central catheter (PICC)
Treatment for:
Venous access
Why it’s done:
PICCs provide intermediate-term (1 week to 2 months) central venous access for treatments such as chemotherapy, TPN, or antibiotics, and can be used for blood draws.
How it’s done:
An interventional radiology nurse practitioner or physician uses ultrasound to access one of the veins in the arm, and the catheter is passed centrally into the vein until the tip lies in the central veins near the heart. PICCs are non-tunneled catheters.
Level of anesthesia:
Local anesthesia only
Risks:
Small risk of bleeding, infection or arrhythmia. Clot may form around the catheter in the arm vein or central vein, and may require catheter removal and/or anticoagulation.
Post-procedure:
No bed rest required. The catheter may be used immediately.
Follow-up:
With referring physician. If problems with the catheter occur, contact the PICC team.
Port catheter placement
Treatment for:
Venous access
Why it’s done:
Port catheters (or Port-a-caths, or ports) provide long-term central venous access for treatments such as chemotherapy, TPN, or antibiotics, and can be used for blood draws. Unlike other types of catheters, ports are entirely under the skin, which makes them less prone to infection, allows for bathing and swimming, and makes them less conspicuous to others.
How it’s done:
An interventional radiologist uses ultrasound to access the target vein, most commonly the internal jugular vein in the neck. X-rays are then used to guide placement of the catheter so that the tip lies in the central veins near the heart. The catheter is tunneled beneath the skin and is connected to a port in the upper chest, which is inserted using a small incision. The port lies beneath the skin and can be accessed through the skin using a special needle.
Level of anesthesia:
Conscious sedation
Risks:
Small risk of bleeding or infection. The port or catheter can sometimes break or clog, necessitating replacement.
Post-procedure:
One to three hours in recovery, then discharge home. The port can be used immediately.
Follow-up:
A wound check is typically performed one week after the procedure in interventional radiology clinic. If problems with the catheter occur, contact your interventional radiologist.
For More Information:
For more information or to schedule an appointment with one of our IR physicians, please call 310-481-7545.