Cushing's Disease
Find your care
We treat pituitary tumors using the latest innovations in minimally invasive procedures. To connect with an expert in the pituitary tumor program, call 310-825-5111.
Cushing's disease is a serious condition of an excess of the steroid hormone cortisol in the blood level caused by a pituitary tumor secreting adrenocorticotropic hormone (ACTH). ACTH is a hormone produced by the normal pituitary gland. ACTH stimulates the adrenal glands (located on top of the kidneys) to produce cortisol, commonly referred to as the stress hormone.
Cushing's Disease: Expert Care in Southern California

Our comprehensive approach to diagnosis and treatment of Cushing's disease sets the UCLA Pituitary Tumor Program apart. Our physicians treat a high volume of patients every year and perform over 100 pituitary surgeries a year, making us one of the top programs in the United States.
Learn more about Cushing's disease:
Cushing's Disease: Physiology
Cushing's disease is rare, affecting 10 to 15 people per million each year, most commonly adults between 20 and 50 years of age. Women account for more than 70 percent of cases.
Most patients with Cushing's disease have small tumors (pituitary microadenomas). However, it can be difficult to diagnosis Cushing's disease, and the diagnosis is often delayed. An endocrinologist should always supervise the evaluation for Cushing's disease. At the UCLA Pituitary Tumor Program, our specialists have years of experience diagnosing and managing Cushing's disease.
Cushing's Disease: Understanding Normal Cortisol Physiology
Cortisol affects the body in many ways, including:
- Maintaining normal blood pressure; inadequate cortisol production is usually associated with low blood pressure.
- Response to stress situations. Cortisol is one of the "fight or flight" hormones.
- An increased blood level of cortisol is essential for you to be able to cope with acutely stressful situations, including surgery.
- Inadequate cortisol release can be fatal.
The adrenal glands produce cortisol in varying amounts throughout the day:
- Blood and saliva cortisol levels are very low at midnight.
- Blood cortisol levels are usually highest in the early morning.
Cushing's Disease vs. Cushing's Syndrome
Cushing's disease is not the same as Cushing's syndrome. Cushing's syndrome refers to the general state characterized by excessive levels of cortisol in the blood and may require different treatments. Elevated cortisol levels can occur for reasons other than a pituitary tumor, including:
- Tumors of the adrenal glands producing cortisol
- Certain types of cancer, elsewhere in the body, can make ACTH, which then stimulates the normal adrenal glands to make excessive cortisol. This is called ectopic ACTH production.
Cushing's syndrome is much more common than Cushing's disease. The most common cause of elevated cortisol levels is taking medications that have cortisol, including: hydrocortisone, prednisone pills, skin ointments, asthma inhalers and joint steroid injections
Less common causes of elevated cortisol levels include:
- An adrenal tumor
- "Pseudo-Cushing's," chronically elevated levels of cortisol due to: depression, alcohol abuse, anorexia nervosa or high estrogen levels
Patients with "pseudo-Cushing's" may be difficult to distinguish from those with true Cushing's. Your doctor may need to order specialized hormonal tests to clarify the diagnosis.
Cushing's disease is used exclusively to describe the condition of excessive cortisol arising from a pituitary tumor secreting the hormone ACTH.
Cushing's Disease: Symptoms
The symptoms related to Cushing's disease and Cushing's syndrome are the same, since both are related to an excess of cortisol. Cushing’s disease symptoms may include:
- Changes in physical characteristics of the body
- Fullness and rounding of the face (so-called "moon facies")
- Added fat on back of neck (so-called "buffalo hump")
- Easy bruising of the skin
- Purplish stretch marks on the abdomen (abdominal striae)
- Excessive weight gain, most marked in the abdominal region, while the legs and arms remain thin
-

Red cheeks ("plethora")
- Excess hair growth on the face, neck, chest, abdomen and thighs
- Generalized weakness and fatigue; wasting of muscles, most noticeably in the upper thighs (You may have difficulty getting up from a chair)
- Menstrual disorders
- Decreased fertility and/or sex drive
- High blood pressure that is often difficult to treat
- Diabetes mellitus, often severe
- Mood and behavior disorders; some patients have psychiatric disorders that require hospitalization
Although uncommon, some patients with Cushing's disease have large pituitary tumors (macroadenomas). In addition to the severe hormonal effects related to increase blood cortisol levels, the large tumor can compress adjacent structures leading to:
-

Vision loss
- When large pituitary adenomas (macroadenomas) grow upward into the brain cavity, the tumor can elevate and compress the optic chiasm, the part of the brain where the optic nerves partially cross.
- A loss of the outer peripheral vision occurs, called a bitemporal hemianopsia
When severe, a patient can only see what is directly in front of them. Many patients do not become aware of their visual loss until it is quite severe.
- Other visual problems can include:
- Loss of visual acuity (blurry vision), especially if the macroadenoma grows forward and compresses an optic nerve.
- Inability to perceive colors as brightly as usual
- Increased compression of the normal gland can cause hormone insufficiency, called hypopituitarism. The symptoms depend upon which hormone is involved.
- Reduction of sex hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- In men, this can lead to a low testosterone level, causing decreased sexual drive and impotence.
- In some cases, there can be loss of body and facial hair.
- In women, this can lead to infertility.
- Large pituitary tumors can slightly elevate blood prolactin levels. Doctors think this occurs because of compression of the pituitary stalk, the connection between the brain and the pituitary gland. It is called the "stalk effect."
- In premenopausal women, this can lead to reduction or loss of menstrual periods and/or breast milk production (galactorrhea).
- Prolactin levels are only slightly elevated, as opposed to prolactinomas in which the prolactin level is usually very high.
- Reduction of sex hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Cushing's Disease: Diagnosis
The early stages of Cushing's disease may be difficult to recognize, especially because the body changes develop slowly. Comparing old and recent photographs often shows the changes in facial appearance and physical characteristics of the body.
The diagnosis may be difficult to make because sometimes the hormone elevations come and go: so called "cyclic" or "periodic" Cushing's disease.
In pregnant women, the pregnancy may worsen the Cushing’s disease symptoms.
Your doctor will conduct a thorough physical exam and ask you about your symptoms and medical history. In general, the first step in making the diagnosis is establishing a state of excessive blood cortisol (i.e. Cushing's syndrome). Assuming cortisol intake is excluded, this typically is done by hormone testing. After this diagnosis is established, an MRI is obtained to determine if a pituitary tumor is visible.
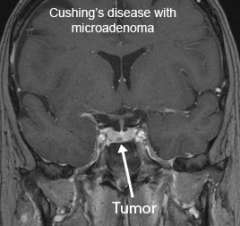
In Cushing's disease, typically very small (microadenoma) tumors are found. If no tumor is visible, then inferior petrosal sinus sampling is indicated (see below).
Tests include:
Hormone testing
The testing for excessive cortisol levels can be complex and challenging. Blood tests may not detect the presence of excessive cortisol secretion because blood levels of cortisol naturally vary throughout the day. Therefore a simple measurement of the blood cortisol level is usually not definitive. Tests we will order include:
- 24-hour urine free cortisol (UFC) measurement
- Cortisol saliva testing
- Blood ACTH
- If low, may suggest the presence of an adrenal tumor producing cortisol

24-hour urine free cortisol (UFC) measurement
The amount of cortisol found in urine collected over a 24-hour period is an important measurement in diagnosing Cushing's syndrome. This test sums the total daily production of cortisol.
- In Cushing's disease, the 24-hour urine free cortisol (UFC) levels are typically at least four to five times greater than normal.
- Your doctor may need two or more elevated 24-hour UFC tests to confirm the diagnose Cushing's syndrome.
- Uncommonly, Cushing's disease can come and go ("periodic Cushing's disease"), requiring multiple 24-hour UFC tests.

Cortisol saliva testing
In some cases, an endocrinologist may request testing for the level of cortisol in the saliva. Similar to blood cortisol levels, the amount of cortisol in the saliva at or near midnight is expected normally to be very low. Multiple elevated midnight salivary cortisol levels may help confirm the diagnosis of Cushing's syndrome.
It is important not brush the teeth just prior to collecting the sample.
This test may not be valid in smokers.
MRI imaging
Once your doctor suspects Cushing's disease based on clinical findings and hormonal testing, a magnetic resonance imaging (MRI) scan of the pituitary gland is the best way to detect the presence of an adenoma in Cushing's disease.
MRI detects a pituitary adenoma in about 70 percent of cases. It is important that you undergo these imaging tests at a pituitary center with special expertise in imaging small tumors. At the UCLA Pituitary Tumor Program, we use powerful 3T (Tesla) MRI scanners that may offer improved chances of identifying very small tumors.
At UCLA, our neuroradiologist personally oversees the MRI scan as it is being acquired in order to perform the optimal scanning sequences to detect tiny pituitary tumors not seen elsewhere.
Inferior petrosal sinus sampling
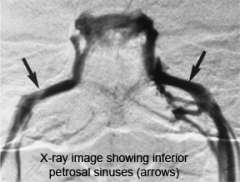
In some cases, MRI fails to identify an abnormality. If your doctor suspects Cushing's disease, he or she may order super-selective inferior petrosal sinus sampling (IPSS).
IPSS must be performed by an experienced interventional neuroradiologist because it carries risk, and if done inappropriately, can give misleading results.
The inferior petrosal sinuses are veins that occur on both sides of the pituitary gland.
- Blood leaving the right half of the pituitary gland drains into the right inferior petrosal sinus and vice versa.
- Specially trained interventional neuroradiologists can thread a tiny catheter into the inferior petrosal sinus. Blood samples are then taken from each sinus and from a vein just below the heart.
If the ACTH level is the same in the inferior petrosal sinus compared to the vein below the heart, this suggests that a tumor somewhere else in the body (ectopic, not pituitary) is producing ACTH.
In Cushing's disease, the ACTH level in the inferior petrosal sinus is much higher compared to the vein below the heart
Cushing's Disease: Other testing
If IPSS testing is not available, other tests include a dexamethasone suppression test. Dexamethasone is a powerful drug that acts similar to, but is more potent than cortisol. This type of testing can suggest either a pituitary or ectopic tumor, but is not as conclusive as IPSS.
Learn more about hormone testing at the UCLA Pituitary Tumor Program.
Cushing's Disease: Treatment Options
Treating Cushing's disease requires an experienced team of experts. To achieve the best outcome, you should seek treatment at a hospital that has a dedicated pituitary tumor program.
Treatment options include:
Surgery for Cushing's Disease

Surgically removing the pituitary adenoma offers the only long-term cure of Cushing's disease.
- When an experienced pituitary surgeon performs the operation, the cure rate for smaller tumors (microadenomas) is 80 percent to 85 percent. If the tumor spread into nearby internal structures, the cure rate is 50 percent to 55 percent.
- Neurosurgeons who specialize in pituitary tumor surgery utilize a technique that removes the tumor as one piece. They find the tumor and dissect it around the edge.
- The endoscopic endonasal approach is a minimally invasive approach, using your natural nasal passageway. It does not require a head incision. Our neurosurgeons have the advanced training and extensive experience necessary for performing this complex procedure.
- An endoscopic technique can be very effective in safely removing tumor, while at the same time minimizing hospitalization time and discomfort.
Medical Therapy for Cushing's Disease
There is no effective drug that lowers ACTH production and shrinks the pituitary tumor. There are medications that inhibit the adrenal gland's production of cortisol. In some patients, these medications can effectively reduce the symptoms related to excessive cortisol when:
- Surgery fails to completely remove the tumor.
- Medication is necessary before surgery, in a patient who is very ill.
Radiation Therapy for Cushing's Disease

In some cases, surgeons may not be able to remove the tumor surgically. Radiation therapy can be very effective in controlling the growth of these tumors.
Stereotactic radiosurgery is a technique in which a highly focused of radiation can be delivered to the tumor target. Because the radiation beam is carefully sculpted, the surrounding brain structures receive only a fraction of the radiation dose and are typically unharmed (with the exception of the normal pituitary gland).
A consequence of radiation treatment is that it can cause delayed pituitary failure. This typically occurs several years after treatment, and therefore continued long-term follow-up with an endocrinologist is important. Hormone replacement may be required.
Other Treatment Options
If the tumor cannot be removed surgically and does not respond to medication or radiation, your doctor may recommend removing the adrenal glands (bilateral adrenalectomy), or BLA. If you undergo BLA:
- You will need replacement of cortisol with hydrocortisone or prednisone after the surgery.
- You must wear a medical alert bracelet or necklace.
- Rapid tumor growth can occur (Nelson's syndrome), since BLA does not affect the pituitary tumor growth.
Cushing's Disease: Clinical Trials
The UCLA Pituitary Program offers clinical trials for the treatment of Cushing's disease.
Contact Us
To schedule an appointment with one of our physicians at the Pituitary Tumor Program, please call (310) 825 5111.
You can also email us at [email protected]