Stroke (Brain Attack)
Find Your Care
Radiologists are experts in all types of imaging, including advanced techniques.
Call today to find medical imaging near you and schedule your imaging procedure (MR, CT, PET, Dexa, Ultrasound).
What is a stroke?
Stroke is the third leading cause of death and the leading cause of adult disability. By definition, a stroke is an interruption of the blood supply to any part of the brain. It is also referred to as a brain attack. If blood flow was stopped for longer than a few seconds and the brain cannot get blood and oxygen, brain cells can die, and the abilities controlled by that area of the brain are lost.
Types of strokes: ischemic stroke and hemorrhagic stroke
An ischemic stroke is caused by a blood clot that blocks an artery and cut off blood flow to the brain. A hemorrhagic stroke is caused by the breakage or "blowout" of a blood vessel in the brain. The ischemic stroke is by far the most common type of stroke.
What are the signs of a stroke?
Patient recognition of an acute stroke is vital, as every second after vessel blockage results in more brain tissue dying. The National Stroke Association recommends remembering the term F.A.S.T. This stands for Face, Arms, Speech and Time.
Act F.A.S.T.
If you suspect someone may be having a stroke, ask the person to do the following:
FACE - Ask the person to smile. Does one side of the face droop?
ARM - Ask the person to raise both arms. does one arm drift downward?
SPEECH - Ask the person to repeat a simple sentence. Are the words slurred? Can the person repeat the sentence correctly, or is he/she has difficulty understanding?
TIME - If the person shows any of these symptoms, time is important. Call 9-1-1 and get to the hospital immediately.
Stroke symptoms
If you have any of the following symptoms, immediately call 9-1-1:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance and coordination
- Sudden severe headache with no known cause.
If you or someone with you has any of these signs, immediately call 9-1-1 or the emergency medical services number. Check the time so you'll know when the first symptom appeared. This information is important to your healthcare provider and can affect treatment decisions.
Who is at risk for stroke?
Anyone can have a stroke, even if you aren't feeling sick. Many stroke risk factors don't have any symptoms. The best way to prevent a stroke is to reduce your controllable risk factors, as 80% of strokes are preventable.
Controllable stroke risk factors
- High Blood Pressure: A blood pressure reading of 140/90 or above increases stroke risk 4-6 times.
- High Cholesterol: High levels of cholesterol in the bloodstream can clog arteries and cause a stroke or heart attack.
- Diabetes: Diabetes increases stroke risk 2-4 times.
- Atrial Fibrillation (AF): Irregular heartbeats increase stroke risk up to six times.
- Tobacco Use/Smoking: Smoking doubles the risk of stroke.
- Alcohol Use: Drinking more than two drinks per day may increase stroke risk by 50%.
- Physical Inactivity or Obesity: Excess weight puts a strain on the entire circulatory system. It also makes people more likely to have high cholesterol, high blood pressure and diabetes — all of which can increase your risk for stroke.
Uncontrollable risk factors
- Age: Your risk of stroke increases with age. After the age of 55, your stroke risk doubles for every decade.
- Gender: Stroke is more common in men than women, but more women than men die from stroke.
- Race: If you are African American, your risk is twice the rate for Caucasians. If you are Hispanic or Asian/Pacific Islander, your stroke risk is also higher than Caucasians.
- Family History: If someone in your family has had a stroke, you have a higher risk of stroke yourself.
- Previous Stroke or Transient Ischemic Attack: If you have already had a stroke or a transient ischemic attack (ministroke), you have a 25-40% chance of having another stroke in the next five years.
What are the treatments for acute stroke?
When it comes to stroke treatment, time is of the essence. Stroke awareness for both the patient and patient's family is the first and most important step to effective treatment. Stroke treatment can be more effective if given quickly, within the first few hours from stroke onset.
Our ability to successfully stop and reverse the devastating effects of acute stroke is limited by the length of time that the brain blood vessels have been blocked. Some stroke treatments can only be used very early after the onset of symptoms, but nearly all of our interventional treatments need to be started before eight hours, except in special circumstances.
IV-rtPA
Intravenous tissue plasminogen activator
Up to three hours, the mainstay of treatment is intravenous tissue plasminogen activator (IV-rtPA). This is an infusion in the vein of a drug which helps dissolve blood clot in acute stroke. However, some patients may not be candidates for this treatment because of other blood clotting problems, recent surgery or other reasons. We can only do this up to three hours, as the risk of bleeding increases after that point. This treatment is also not always effective. In those patients and in patients up to eight hours, we will then try to go into the artery to open up the blockage with other techniques.
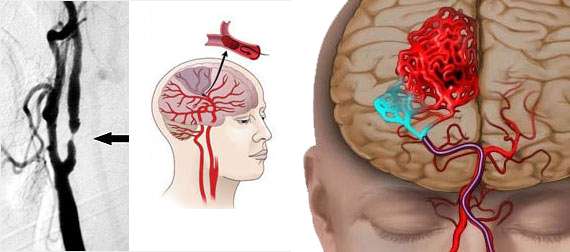
Mechanical Devices
MERCI clot retrieval system, and the Penumbra Clot aspiration system.
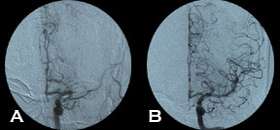
There are two mechanical devices approved by the FDA for use in this situation: they are the MERCI clot retrieval system, and the Penumbra Clot aspiration system.
Both devices are navigated into the blocked brain blood vessel by entering into the artery at the top of the thigh and using X-ray guidance. The MERCI device is a helical snare which grasps the clot and is then pulled out, and the Penumbra device uses aspiration to suction out the clot. In addition, an FDA off-label use of the rTPA to dissolve the blood clot is done by injecting the drug directly into the clot at a lower dose using the same catheterization techniques.
With advanced brain imaging, we often select patients for treatment not by time, but by the physiological status of the brain tissue. Our modern CT and MRI techniques can tell us if there is brain to be saved even after the eight hour window, and we will apply some of the treatments beyond 8 hours in appropriate patients.
But, the bottom line is to know what the signs of stroke are and get to the hospital quickly. Even if no acute revascularization procedure is performed, the medical care at a stroke center significantly improves outcomes.
Quick links
- Patient Story: Understanding & Surviving a Stroke
- Interventional Neuroradiology
- MERCI Retriever
- Patient Referrals
- Schedule an Interventional Radiology Consultation
- Our Locations