Pulmonary Arteriovenous Malformations (AVM)
Find your care
Our board-certified physicians diagnose and treat many vascular conditions. Call 310-481-7545 to learn more about interventional radiology services.
What is a pulmonary arteriovenous malformation (AVM)?
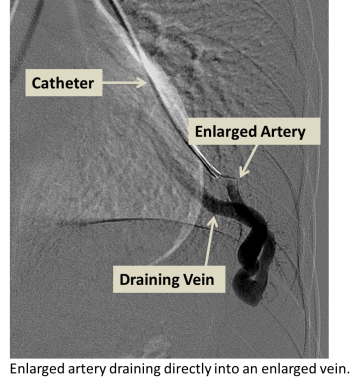
Arteriovenous malformations (AVMs) refer to arteries and veins with abnormal connections between them. In the lungs, arteries first carry blood from the heart to smaller arteries which then feed into even smaller vessels called capillaries. Capillaries, which are within organs, slow down blood flow and allow for nutrient and gas exchange between the blood and organs. Veins carry blood away from capillaries and back to the heart.
In the presence of an AVM, the arteries and veins are directly connected without intervening capillaries, reducing gas exchange and causing decreased oxygen levels and shortness of breath, especially with exertion. The abnormal arteries and veins in an AVM often have weak walls, and bleeding into the lung can result. Clots or bacteria in the lung circulation that would normally get trapped in small capillaries can pass through the AVM to the blood vessels of the brain and cause stroke or brain abscess.
Risk Factors
AVMs can be solitary or multiple when they occur as part of a syndrome such as HHT. AVMs can develop during fetal development or soon after birth, although the causes are not known. Certain types of AVMs can occur after penetrating trauma such as stab wounds or projectile injuries. Most AVMs are not inherited, but AVMs may occur as part of heritable genetic diseases such as Hereditary Hemorrhagic Telangiectasia (HHT).
Symptoms
Symptoms vary and many patients with pulmonary AVM are asymptomatic. With larger or multiple pulmonary AVMs, shortness of breath may be present, especially with exertion. Stroke or brain abscess can occur at any time. The AVM may bleed, causing coughing of blood or collections of blood around the lung.
Diagnosis
- Bubble study (Microbubbles injected into an IV while an ultrasound monitors the heart or outflow arteries; normally these microbubbles will be filtered out by the lung, but if a lung AVM is present then the bubbles will pass through the AVM and be detected by the ultrasound)
- CT angiography (Performed if bubble study is positive; allows enumeration and measurement of lung AVMs and determines if treatment is required)
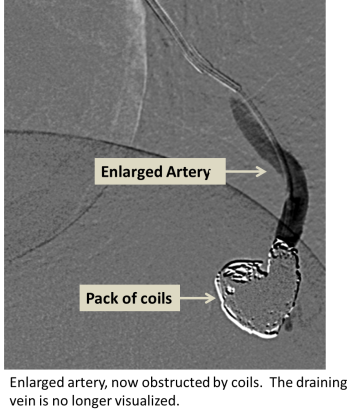
- Angiography (X-ray with contrast agent to visualize and treat the abnormal blood vessels)
Treatments
- Pulmonary AVM embolization
For More Information:
For more information or to schedule an appointment with one of our IR physicians, please call 310-481-7545.