Thyroid and Parathyroid Disease
Find your care
We deliver effective, minimally invasive treatments in a caring environment. Call 310-267-7838 to connect with an expert in endocrine surgery.
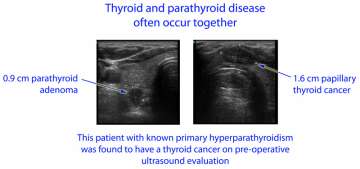
Parathyroid Disease and Thyroid Disease Commonly Occur Together
Patients with Both Thyroid and Parathyroid Disease
Importance of ultrasound evaluation of the thyroid and parathyroid glands prior to surgery
We have previously mentioned that patients with parathyroid disease (such as primary hyperparathyroidism) should seek treatment at endocrine surgery centers with expertise in both thyroid and parathyroid conditions (see Frequently asked questions about parathyroid surgery). The reason for this is that both parathyroid disease and thyroid disease are highly prevalent (common) in women over 45 years of age, and thus the two conditions often overlap in individual patients. Primary hyperparathyroidism and thyroid cancer affect women 3-4 times as often as men. Primary hyperparathyroidism affects up to 3% of post-menopausal women. About half of women aged 45 and older have thyroid nodules, and approximately 4% of these nodules will turn out to be malignant (cancerous). Recent research shows that thyroid cancer rates have tripled in the United States since the 1970s (see Surgery for thyroid cancer)

For this reason, it is our opinion that every patient being evaluated for parathyroid disease should undergo ultrasound evaluation of the thyroid and parathyroid glands prior to surgery.
Ideally this should be done by the surgeon during the initial consultation, or planning phase for surgery. This is our standard practice at UCLA Endocrine Surgery, and it is rapidly gaining wide acceptance among other expert centers (see References). An important study conducted at the University of Wisconsin showed that almost half of patients being evaluated for primary hyperparathyroidism had suspicious thyroid findings on ultrasound. Thyroid cancer was discovered in several patients, allowing for appropriate treatment of both thyroid and parathyroid disease with a single operation. Experts at the Cleveland Clinic conducted a similar study in which they found that routine pre-operative ultrasound evaluation actually reduced the need for unnecessary thyroid surgery.
Let’s take a moment to understand these two research findings a little better. Ultrasound allows thyroid cancer to be detected in a small but significant number of patients being evaluated for parathyroid disease (primary hyperparathyroidism). Those patients are at risk for inadequate initial surgery, i.e. if the thyroid cancer was missed the first time, those patients would potentially need a second operation to treat thyroid cancer. Given how frequently parathyroid disease and thyroid cancer occur together, it is statistically inevitable that solely operating on the parathyroids without ultrasound evaluation of the thyroid will lead to thyroid cancers being left behind untreated. On the other hand, many thyroid nodules are benign and do not require surgery. Those patients are at risk for excessive surgery, for example if their surgeon discovers a thyroid nodule at the time of surgery and decides to remove the nodule or biopsy it surgically, which is often not the right thing to do (Why? See below).
When it comes to any type of surgery, what patients need is not too little surgery, nor too much surgery. Patients need just the right amount of surgery. Ultrasound permits this in thyroid and parathyroid disease by creating a roadmap for the operation. We would not contemplate performing this type of surgery without ultrasound guidance; in our opinion that would be tantamount to “flying blind” in the neck.
It is common for many surgeons to offer to inspect or evaluate the thyroid during parathyroid surgery. We do not believe this represents best clinical practice, for several reasons.
Why ultrasound evaluation of the thyroid prior to parathyroid surgery is preferable to visual inspection of the thyroid during parathyroid surgery
- Visual inspection of the thyroid during parathyroid surgery may only reveal problems on the surface of the thyroid, as opposed to ultrasound which can penetrate into the deep substance of the thyroid.
- The discovery of a suspicious thyroid nodule during parathyroid surgery may lead to enucleation (also known as nodulectomy or surgical/open biopsy) of the thyroid nodule. This is not considered standard of care for suspicious thyroid nodules. Suspicious thyroid nodules are best treated with thyroid lobectomy (hemithyroidectomy or removal of half of the thyroid gland). Lobectomy permits pathologic (microscopic) evaluation of the boundary between the suspicious nodule and the adjacent normal thyroid tissue, which often reveals the deciding factor between which nodules are malignant (cancerous) and which nodules are benign, that is, the presence or absence of invasion.
- The presence of thyroid cancer is best detected by pre-operative ultrasound-guided fine-needle aspiration (FNA) of thyroid nodules. This is widely accepted as best practice. Having this knowledge in advance of surgery permits careful planning of the operation and mobilization of any additional resources necessary for a more complex cancer operation. Thyroid cancer surgery generally involves a total thyroidectomy and often a lymph node dissection. It is best for the surgeon to be prepared for this ahead of time, as an improvised thyroid cancer operation is unlikely to yield the best outcome for the patient.
- Ultrasound affords the patient the best chance of having a single, definitive operation. We have previously discussed the potential for leaving thyroid cancers behind. Indeed, we see patients for re-do thyroid surgery every week at UCLA and sometimes we perform multiple re-do thyroid operations in a single day. Re-do surgery is associated with risks that are several fold higher than initial neck surgery, and hence re-do surgery should be avoided whenever possible.
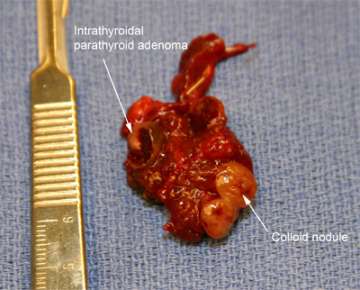
Specimen from a patient with both thyroid and parathyroid disease.
Intrathyroidal parathyroid adenomas (parathyroid tumors lodged within the substance of the thyroid gland) are found in about 1% of humans. This patient's thyroid nodule was determined to be benign.
All of the above points are common sense. Before embarking on a neck operation, the surgeon should have complete knowledge of everything that is going on in the neck (the roadmap we discussed above). This is just “doing one’s homework” in preparation for surgery, and certainly you deserve this level of quality and detail-oriented evaluation in your health care. Ultrasound permits avoidance of almost all surprises or “spur of the moment” decision-making during surgery. Now, obviously not everything can be anticipated, and surgery will always require surgeons to think well on their feet in the best interest of their patients. However, with routine use of pre-operative ultrasound, we have been able to reduce the number of even minor unanticipated events to less than 5% during thyroid and parathyroid surgery. We don’t like surprises. In this sense, having surgery is a lot like taking a commercial air flight – the best possible experience is one with no surprises and no excitement (learn more about Health care quality and safety).
In summary, we recommend that all patients being evaluated for parathyroid surgery undergo routine ultrasound examination of the thyroid and parathyroid glands by a surgeon experienced in both thyroid and parathyroid surgery. Careful planning of the operation in advance will maximize the likelihood of a good outcome.
References
- Coker LH, Rorie K, Cantley L, Kirkland K, Stump D, Burbank N, Tembreull T,Williamson J, Perrier N. Primary hyperparathyroidism, cognition, and health-related quality of life. Ann Surg. 2005 Nov;242(5):642-50. Review. PubMed PMID: 16244536; PubMed Central PMCID: PMC1409861.
- Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med. 2004 Oct 21;351(17):1764-71. Review. PubMed PMID: 15496625.
- Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006 May 10;295(18):2164-7. PubMed PMID: 16684987.
- Harari A, Mitmaker E, Grogan RH, Lee J, Shen W, Gosnell J, Clark O, Duh QY. Primary hyperparathyroidism patients with positive preoperative sestamibi scaand negative ultrasound are more likely to have posteriorly located upper gland adenomas (PLUGs). Ann Surg Oncol. 2011 Jun;18(6):1717-22. Epub 2011 Jan 5. PubMed PMID: 21207169; PubMed Central PMCID: PMC3087871.
- Morris LF, Ragavendra N, Yeh MW. Evidence-based assessment of the role of ultrasonography in the management of benign thyroid nodules. World J Surg. 2008 Jul;32(7):1253-63. Review. PubMed PMID: 18311500.
- Morris LF, Zanocco K, Ituarte PH, Ro K, Duh QY, Sturgeon C, Yeh MW. The value of intraoperative parathyroid hormone monitoring in localized primary hyperparathyroidism: a cost analysis. Ann Surg Oncol. 2010 Mar;17(3):679-85. Epub 2009 Nov 3. PubMed PMID: 19885701; PubMed Central PMCID: PMC2820694.
- Hwang RS, Morris LF, Ro K, Park S, Ituarte PH, Hong JC, Yeh MW. A selective, Bayesian approach to intraoperative PTH monitoring. Ann Surg. 2010 Jun;251(6):1122-6. PubMed PMID: 20485138.
- Yeh MW, Barraclough BM, Sidhu SB, Sywak MS, Barraclough BH, Delbridge LW. Two hundred consecutive parathyroid ultrasound studies by a single clinician: the impact of experience. Endocr Pract. 2006 May-Jun;12(3):257-63. PubMed PMID: 16772196.
- Barraclough BM, Barraclough BH. Ultrasound of the thyroid and parathyroid glands. World J Surg. 2000 Feb;24(2):158-65. Review. PubMed PMID: 10633142.
- Miller BS, Gauger PG, Broome JT, Burney RE, Doherty GM. An international perspective on ultrasound training and use for thyroid and parathyroid disease. World J Surg. 2010 Jun;34(6):1157-63. PubMed PMID: 20162277.
- Adler JT, Chen H, Schaefer S, Sippel RS. Does routine use of ultrasound result in additional thyroid procedures in patients with primary hyperparathyroidism? J Am Coll Surg. 2010 Oct;211(4):536-9. Epub 2010 Jul 31. PubMed PMID: 20822743.
- Milas M, Stephen A, Berber E, Wagner K, Miskulin J, Siperstein A. Ultrasonography for the endocrine surgeon: a valuable clinical tool that enhances diagnostic and therapeutic outcomes. Surgery. 2005 Dec;138(6):1193-200; discussion 1200-1. PubMed PMID: 16360408.
- Milas M, Mensah A, Alghoul M, Berber E, Stephen A, Siperstein A, Weber CJ. The impact of office neck ultrasonography on reducing unnecessary thyroid surgery in patients undergoing parathyroidectomy. Thyroid. 2005 Sep;15(9):1055-9. PubMed PMID: 16187914.
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid.
- 2009 Nov;19(11):1167-214. Erratum in: Thyroid. 2010 Aug;20(8):942. Hauger, Bryan R [corrected to Haugen, Bryan R]. Thyroid. 2010 Jun;20(6):674-5. PubMed PMID: 19860577.