Quality Improvement and Clinical Innovation



The Quality Improvement and Clinical Innovation Committee, chaired by Dr. Michelle Hickey, is focused on integrating quality themes into the clinical, operational and educational efforts of the faculty and staff of the Department of Pathology and Laboratory Medicine. Quality improvement projects are ongoing throughout all areas of the laboratory that support the MOVERS quality vision of UCLA Health. The department has a large footprint in clinical service with over 6 million tests (3.1 million inpatient tests) performed annually and over 200,000 surgical pathology/cytology cases annually. With 74 faculty, 22 residents, and over 500 staff involved in hospital and research activities, we are committed to transformational change through value-based care redesign and quality improvement research.

Chair, Quality Improvement and Clinical Innovation Committee
Committee Members
Alexander Nobori, MD
Jamar P. Uzzell, MD
Sofia Hwang, MD
Jitin Makker, MD
Amanda Fakih, MFA
Nikki Salami
Project Snapshots

Resident Education Quality Improvement
The purpose of REQIPP (Resident Education Quality Improvement Program - Pathology & Laboratory Medicine) is to actively engage residents and fellows in the evaluation and development of the pathology and laboratory medicine quality improvement programs while facilitating the departments’ quality improvement priorities. Our trainees are encouraged to participate in both departmental and multidisciplinary projects. The program will assist in the identification of new quality improvement initiatives in an effort to standardize care and improve outcomes for UCLA patients all while achieving the ACGME and ABP Pathology Milestones.
The programs curriculum includes QStream a quality improvement focused mobile software implemented for UCLA Housestaff and focused lecture series.
Our trainees also have the opportunity to present their QI projects during our annual Quality and Clinical Innovation Day. Abstract submission and publication are also encouraged.
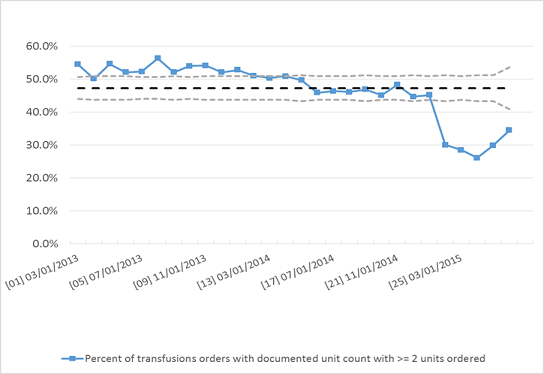
RBC Utilization
Our goal is to standardize transfusion practices, reduce routine 2U RBC orders and avoid transfusion at Hb ≥ 8g/dL in stable patients.
Our strategy is to implement CPOE best practice alerts (BPA) triggered based on patient Hgb and physician order, provide timely, data-driven feedback and targeted education, and forming a multi-disciplinary team consisting of hospitalists, transfusion medicine (transfusion safety officer), nursing, and IT.
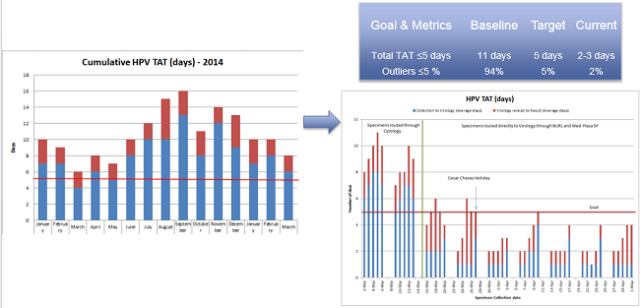
HPV Turn Around Time (HPV TATs)
By streamlining our process for specimen hand-offs and aliquoting, we have been able to significantly reduce the TATs on HPV testing.
Quality Improvement through Electronic Crossmatch
UCLA uses the electronic crossmatch (EXM) as a safe and efficient alternative to a serologic crossmatch method to ensure ABO compatibility for patients with no previous or current history of clinically significant antibodies. Following implementation of CareConnect and computerized physician order entry (CPOE), the blood bank observed inefficiencies associated with increased duplicate and excess orders where many blood units prepared were never requested (issued) for transfusion. To address the workload and blood inventory constraints associated with these inefficiencies, we implemented a new policy where orders from patients eligible for EXM are pended until actual issue requests were received. This policy reduced the number of crossmatched units that were never issued from 840 to 300 units/month, improved work place efficiency and improved inventory management, while maintaining clinically acceptable issue turn-around-time.
Quality in the Ambulatory Point–of–Care (POC) Testing program
Point of Care (POC) tests are laboratory tests performed directly in the physician office and are of extreme value in providing an immediate result that can be directly acted upon by the provider. These tests are built to be easy to perform, however still require quality control to ensure the test kit provides accurate results and that the person performing the test understands the test’s performance limitations. As the majority of POC tests are performed outside of the traditional laboratory setting, the goal of the POC Quality program is to improve quality of the POC testing within the UCLA Health System. This endeavor, in conjunction with Ambulatory Care Nursing, is being implemented through education of test reliability, standardization of POC tests performed, standardization of operator training, and through implementation of quality control guidelines.

RadPath Program
The RadPath program is a collaboration between radiology and pathology. Our goal is to provide an integrated radiology and pathology report. The integrated report provides the following advantages:
- Collaborated findings and coordinated diagnosis.
- Improved information flow downstream to end-user and upstream to diagnosticians.
- Improved speed and accuracy of diagnosis.
- Improved ability of both specialties to develop evidence-based technologies to further the healthcare enterprise.
- Facilitates ease of data retrieval:
- Tumor size, location, clinical stage
- Tumor type, histologic grade
- Molecular profile
For more information about Quality Improvement and Clinical Innovation, contact:
Dr. Michelle Hickey at 310-267-2427.