Pediatric Hydrocephalus Program
Find your care
Call 310-825-5111 to learn more about our world-class pediatric neurosurgery services.
Overview
Hydrocephalus is an abnormal accumulation of cerebrospinal fluid (CSF) within cavities called ventricles inside the brain. It occurs when there is an imbalance between the amount of CSF that is produced and the rate at which it is absorbed.
Watch Video: Management of Pediatric Hydrocephalus
As the CSF builds up, it causes the ventricles to enlarge and the pressure inside the head to increase. Untreated hydrocephalus may result in death or significant neurological and cognitive impairment.

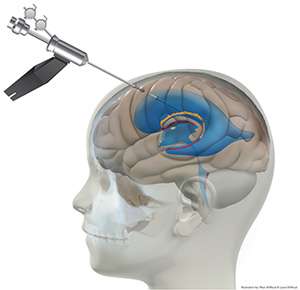
The historic way to treat hydrocephalus is with a shunt. It goes from the ventricle of the brain to the abdominal cavity or another cavity that can absorb CSF. This technology has come since the late 1950s with little progress since that time. Although it works well, it creates a dependence of this implanted device. This device has the highest failure rate from all medically implanted devices often requiring multiple surgeries.
A re-emerging technique combines a procedure developed in the late 1990s, an endoscopic third ventriculostomy, using a very small camera in a minimally invasive manner to make a hole at the floor of the brain to allow CSF to escape, with a new technique called choroid plexus cauterization, which reduces the tissue that creates CSF. This increases the success rate, meaning no further operations required, in about 50-60% of children who have never been treated before for hydrocephalus. Our success rates for hydrocephalus surgery is on par with the top pediatric hospitals across the United States.
Here at UCLA, we are one of the few centers that have special expertise and experience treating children with this new re-emerging technique. Not all children will be good candidates for an ETV and CPC. In those children, we still have the option of treating hydrocephalus with traditional shunt surgery and have available to us the array of the latest shunt technology.
Request an Appointment
Recent Publications
- Social media networking in pediatric hydrocephalus: a point-prevalence analysis of utilization.
Elkarim GA, Alotaibi NM, Samuel N, Wang S, Ibrahim GM, Fallah A, Weil AG, Kulkarni AV.
J Neurosurg Pediatr. 2017 Aug;20(2):119-124. doi: 10.3171/2017.3.PEDS16552. Epub 2017 May 26. - Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization: a propensity score-matched cohort and survival analysis.
Wang S, Stone S, Weil AG, Fallah A, Warf BC, Ragheb J, Bhatia S, Kulkarni AV.
J Neurosurg Pediatr. 2017 May;19(5):585-591. doi: 10.3171/2016.12.PEDS16443. Epub 2017 Mar 17. - Los Angeles Pediatric Society E-Newsletter - August 2016
- Alexander G. Weil, Harrison Westwik, Shelly Wang, Naif M. Alotaibi, Lior Elkaim, George Ibahim, Anthony Wang, Rojine Ariani, Louis Crevier, Bethany Myers, Aria Fallah. Efficacy and safety of endoscopic third ventriculostomy and choroid plexus cauterization for infantile hydrocephalus: a systematic review and meta-analysis. Springer-Verlag Berlin Heidelberg. Jun 2016; DOI 10.1007. Link to abstract >
- Alexander G. Weil, MD, FRCSC, Fallah A., MD, MSc, Parthasarathi Chamiraju, MD, John Ragheb, MD, and Sanjiv Bhatia, MD. Endoscopic third ventriculostomy and choroid plexus cauterization with a rigid neuroendoscope in infants with hydrocephalus. Journal of Neurosurgery Pediatrics. 2015; 10.3171/2015.5.PEDS14692. Link to abstract
Webinars
Modern and Comprehensive Management of Pediatric Hydrocephalus – Aria Fallah