Recurrent pregnancy loss
Find Your Care
Whether you need a preventative examination, pregnancy care or treatment for a gynecological condition, our OB/GYN specialists are here for you.
Call 310-794-7274 to schedule an appointment today.
Recurrent pregnancy loss: symptoms, treatment & diagnosis
What is recurrent pregnancy loss?
If you can get pregnant but keep miscarrying, it is called recurrent pregnancy loss. Recurrent pregnancy loss is classically defined as the occurrence of three or more consecutive pregnancy losses. However, the American Society of Reproductive Medicine (ASRM) has recently redefined recurrent pregnancy loss as two or more pregnancy losses. A pregnancy loss is defined as a clinically-recognized pregnancy involuntarily ending before 20 weeks. A clinically-recognized pregnancy means that the pregnancy has been visualized on an ultrasound or that pregnancy tissue was identified after a pregnancy loss.
What causes recurrent pregnancy loss?
Most pregnancy losses result from chromosomal, or genetic, abnormalities, and are random events. The abnormality may come from the egg, the sperm, or the early embryo. Approximately 12–15% of all clinically recognized pregnancies end in miscarriage. However, it is estimated that at least 30–60% of all conceptions will end within the first 12 weeks of gestation. Up to 50% of the time, the woman doesn’t even realize that she was ever pregnant. The risk of miscarriage increases with the number of previous pregnancy losses, but is typically less than 50%.
Advancing maternal age is associated with an increased risk of miscarriage, which is thought to be due to poor egg quality leading to chromosomal (genetic) abnormalities. Sometimes, the mother or father themselves may have a slight irregularity in their genes, but the offspring could be more severely affected and thus result in miscarriage.
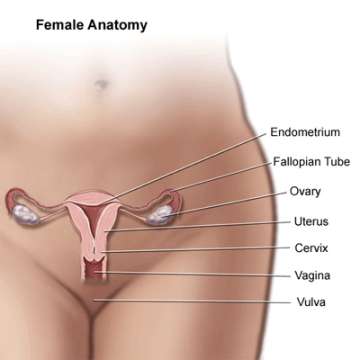
Sometimes, there could be an abnormality in the uterus (the womb) that leads to miscarriage. The miscarriage may be due to poor blood supply to the pregnancy or inflammation. Some women may be born with an irregularly shaped uterus, and some women may develop abnormalities with their uterus over time.
A woman’s immune system may also play a role in recurrent pregnancy loss. Hormone abnormalities may also impact pregnancy loss, including thyroid disease and diabetes. Abnormalities in a mother’s blood clotting may also affect pregnancy loss.
Generally speaking, environmental factors, stress, and occupational factors do not seem to be related to pregnancy loss.
What tests are done for couples with recurrent pregnancy loss?
First, a physician will take a detailed medical, surgical, family, and genetic history and perform a physical examination. Testing that may be done includes karyotype analysis of both partners. The karyotype is the chromosomal, or genetic, make-up of a person. The purpose is to find abnormalities in the parents that could be passed on to the offspring, resulting in miscarriage. Because karyotype abnormalities are relatively rare, a doctor may choose to not perform this test unless other, more common, abnormalities are ruled out.
The uterus (the womb) and the uterine cavity (inside of the womb) will often be evaluated. There are several ways to evaluate the uterine cavity, including an ultrasound, saline ultrasound, hysterosalpingogram X-ray, MRI (magnetic resonance imaging), and/or hysteroscopy (to look inside the uterus). An ultrasound is often done as a first test. The ultrasound can give information about the shape of the uterus and the presence of fibroids (benign round muscle tumors). A saline ultrasound is when fluid is injected into the inside of the uterus so that the physician can see if there are abnormalities with the inside of the uterus, including polyps (growths of the lining of the uterus), fibroids, or scarring. A hysterosalpingogram is an X-ray of the uterus and tubes, and can help a doctor to evaluate not only the inside of the uterus, but also the tubes (whether they are open or not). A hysteroscopy is a minor surgical procedure where a camera is placed through the cervix into the uterus so that the doctor can directly visualize the inside of the uterus. The doctor can also remove polyps and fibroids and can resect a septum or scar tissue, if present. A uterine septum is an abnormality of the shape of the uterus that a woman has since birth. An MRI may be done to evaluate the location of fibroids and in cases of abnormalities of the shape of a uterus.
Antiphospholipid antibodies, particularly anticardiolipin antibody and lupus anticoagulant, will likely be checked. These antibodies are related to the antiphospholipid syndrome, which may be related to pregnancy loss. Any woman with a pregnancy loss at or beyond the 10th week of gestation (with a “normal” appearing fetus) or with three recurrent losses at any gestational age should be screened, according to the American College of Obstetrics and Gynecology (ACOG). Testing for inherited thrombophilias, or abnormally increased blood clotting, is not routinely recommended in women who have experienced recurrent fetal loss because studies have not shown a benefit of giving medicine to prevent clots in these patients. However, testing for abnormal blood clotting should be done if there is a personal history of blood clots associated with risk factors such as surgery, bone fractures, or prolonged immobilization, or if a patient has a parent or sibling with a disorder of excessive blood clotting.
Tests of hormone function may also be done. Thyroid function tests and thyroid antibodies may be checked, along with measurement of prolactin, the hormone responsible for breast milk production. Ovarian reserve tests may be performed, which indicate how well an ovary is functioning. Some studies indicate that poorer ovarian function, as shown by these hormone tests, may be related to chromosomal abnormalities of the eggs in the ovary. Testing for diabetes may be done if a woman is at risk for or has manifestations of diabetes.
What treatment is available for recurrent pregnancy loss?
The treatment recommendations for patients with recurrent pregnancy loss are based on the underlying cause of recurrent pregnancy loss. No matter what the results of the work-up are, the chance for a successful future pregnancy is high: 77% if the work-up showed no abnormalities, and 71% if an abnormality was found.
Individuals in whom a karyotypic (a chromosomal or genetic) abnormality is found are often referred for genetic counseling. There, a specialist can discuss what the genetic abnormality is and the likelihood of having a chromosomally normal or abnormal pregnancy in the future. Some affected couples may choose to undergo prenatal genetic studies during pregnancy to check the genetic make-up of the offspring with either 1) chorionic villus sampling (CVS), in which a piece of placenta is biopsied late in the first trimester or early in the second trimester, or 2) amniocentesis, which removes some of the amniotic fluid (the fluid that surrounds the baby during pregnancy) for analysis. In vitro fertilization (IVF) with preimplantation genetic diagnosis (PGD) can also be done. With this process, the woman takes shots for several days so that many eggs grow in her ovaries. The eggs are then retrieved from the ovaries in a minor surgical procedure. One sperm is then injected into each egg and the embryo is allowed to grow. One cell of the embryo is then biopsied and the genetic make-up is analyzed to avoid the transfer of an affected embryo.
If a uterine abnormality is found, surgery may be performed depending on the defect. If antiphospolipid syndrome is diagnosed, certain medications that reduce blood clot formation may be given. If thyroid dysfunction or diabetes are diagnosed, specific medications can be prescribed.
Unexplained recurrent pregnancy loss
Over 50% of patients with recurrent pregnancy loss will have unexplained recurrent pregnancy loss, which means that no specific cause could be identified in the work-up. Various treatments may be offered to these patients, but there is no universal recommendation for treatment of these patients. Despite this, the overall chance of pregnancy is good, more than 50%, without any intervention at all.