News and Insights
Updates from the UCLA Health Newsroom
Latest News Releases
Resources for Journalists

The UCLA Health Media Relations Office can help credentialed journalists with background, story ideas, and comment from the experts and specialists at UCLA Health's four hospitals and over 200 clinics, the UCLA Health Jonsson Comprehensive Cancer Center and the David Geffen School of Medicine at UCLA.
Stay in Touch
Subscribe to UCLA Health newsletters and publications for the latest developments.
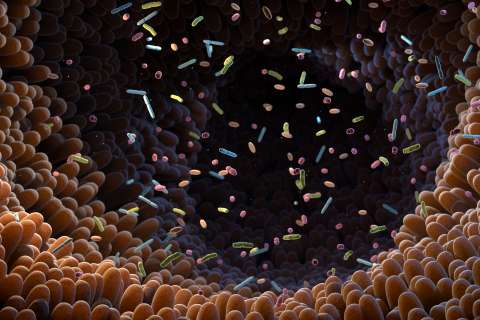
Science and Research




Behavioral Health



Cancer Care




Patient Stories