Infertility
Find Your Care
Whether you need a preventative examination, pregnancy care or treatment for a gynecological condition, our OB/GYN specialists are here for you.
Call 310-794-7274 to schedule an appointment today.
Infertility: Symptoms, Treatment, Diagnosis
Affiliated Physicians: Fertility and Reproductive Health Center | Obstetrics
What is Normal Fertility and When Does it Become Infertility?
What is Infertility?
Most people will have the strong desire to conceive a child at some point during their lifetime. Understanding what defines normal fertility is crucial to helping a person, or couple, know when it is time to seek help. Most couples (approximately 85%) will achieve pregnancy within one year of trying, with the greatest likelihood of conception occurring during the earlier months. Only an additional 7% of couples will conceive in the second year.
As a result, infertility has come to be defined as the inability to conceive within 12 months. This diagnosis is therefore shared by 15% of couples attempting to conceive. We generally recommend seeking the help of a reproductive endocrinologist if conception has not occurred within 12 months. However, there are various scenarios where one may be advised to seek help earlier. These include:
- Infrequent menstrual periods: When a woman has regular menstrual periods, defined as regular cycles occurring every 21 to 35 days, this almost always indicates that she ovulates regularly. Ovulation of the egg occurs approximately 2 weeks before the start of the next period. If a woman has cycles at intervals of greater than 35 days, it may indicate that she is not ovulating an egg predictably, or even at all. Ovulation of the egg is essential for pregnancy. Therefore, we recommend an evaluation if menstrual cycles are infrequent or irregular in a couple attempting pregnancy.
- Female age of 35 years or older: For unclear reasons, egg numbers decrease at a rapid rate as women age. Furthermore, as aging occurs, egg quality, or the likelihood of an egg being genetically normal, decreases. Therefore we recommend a fertility evaluation if a couple has been attempting pregnancy for 6 months or more when the woman is 35 years of age or older.
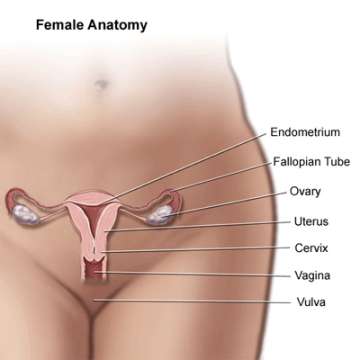
- A history of pelvic infections or sexually transmitted diseases: Sexually transmitted infections, such as chlamydia or gonorrhea, can cause inflammation and permanent scarring of the fallopian tubes. The presence of open tubes is essential for natural conception, as sperm must traverse the tubes in order to reach and fertilize the ovulated egg. We recommend immediate evaluation for a couple attempting pregnancy when the woman has a prior history of pelvic infection. As part of the fertility evaluation, we will perform an HSG, a test designed to evaluate if the fallopian tubes are open.
- Known uterine fibroids or endometrial polyps: Uterine abnormalities, such as fibroids that indent the endometrial cavity and endometrial polyps, can impair how the endometrium (the lining of the uterus) and embryo interact to lower implantation and pregnancy rates. These abnormalities can also cause irregular bleeding between menstrual cycles. Evaluation should be pursued by 6 months of attempted pregnancy in women with a known history of these abnormalities or a history of bleeding between menstrual cycles. The main approach to correcting or removing these uterine abnormalities is by hysteroscopy, a surgical method by which a narrow scope with a camera is placed within the uterine cavity. Instruments can be introduced through the hysteroscope, allowing the surgeon to remove or correct any anatomic abnormalities.
- Known male factor semen abnormalities: If a male partner has a history of infertility with a prior partner, or if there are abnormalities on his semen analysis, then we advise earlier fertility evaluation, ideally within 6 months of attempting pregnancy.
What is Involved in the Fertility Evaluation?
Infertility Tests
History and physical examination – First and foremost, your fertility physician will take a very thorough medical and fertility history. Your doctor may ask you many of the following questions: How long have you been trying to get pregnant? How often are you having intercourse? Do you have pain with menstrual periods or intercourse? Have you been pregnant before? What happened with your prior pregnancies? Have you had any sexually transmitted infections or abnormal pap smears? How often do you have menstrual cycles? Do you have any medical problems or prior surgeries? Do you have a family history of medical problems? These and many other questions will help your physician design a specific evaluation and potential treatment for you. In addition to a careful history, a physical evaluation may also be performed.
Transvaginal ultrasound – Ultrasound is an important tool in evaluating the structure of the uterus, tubes, and ovaries. Ultrasound can detect uterine abnormalities such as fibroids and polyps, distal fallopian tube occlusion, and ovarian abnormalities including ovarian cysts. Additionally, transvaginal ultrasound affords the opportunity for your physician to assess the relative number of available eggs. This measurement is called the antral follicle count and may correlate with fertility potential.
Laboratory testing – Depending on the results of the evaluation discussed above, your physician may request specific blood tests. The most common of these tests include measurements of blood levels of certain hormones such as estradiol and FSH, which are related to ovarian function and overall egg numbers; TSH, which assesses thyroid function; and prolactin, a hormone that can affect menstrual function if elevated.
Hysterosalpingogram (HSG) – This test is essential for evaluating fallopian tubal patency, uterine filling defects such as fibroids and polyps, and scarring of the uterine cavity (Asherman syndrome). Many uterine and tubal abnormalities detected by the HSG can be surgically corrected.
Semen analysis – The semen analysis is the main test to evaluate the male partner. There are four parameters analyzed:
- semen volume – should be at least 1.5 to 2 ml. A smaller amount may suggest a structural or hormonal problem leading to deficient semen production;
- sperm concentration – normal concentration should be at least 20 million sperm per 1 ml of semen. A lower concentration may lead to a lower chance for conception without treatment;
- sperm motility or movement – a normal motility should be at least 50%. Less than 50% motility may significantly affect the ability for sperm to fertilize the egg without therapy; and
- morphology, or shape – there are three parts of the sperm that are analyzed for morphology: the head, midpeice, and tail. Abnormality in any of those regions may indicate abnormal sperm function and compromise the ability of sperm to fertilize the egg. Ideally, using strict morphology criteria, a minimum of 5 – 15% normal forms leads to a better ability for sperm to fertilize the egg. An abnormal semen analysis warrants a further evaluation usually by a reproductive urologist. Your physician will refer you to a reproductive urologist if appropriate.
What are the Common Causes of Infertility?
What Causes Infertility?
1) Advancing maternal age
Historically before the latter 20th century, women were conceiving in their teens and twenties, when age-related abnormalities with the egg were not evident. However, in our modern era, women are delaying child birth until their thirties and forties, which has lead to the discovery of the adverse effect of advanced maternal age on egg function. In fact, female age-related infertility is the most common cause of infertility today. For unknown reasons, as women age, egg numbers decrease at a rapid rate. And as aging occurs, egg quality, or the likelihood of an egg being genetically normal, decreases as well. Hence the ability to conceive a normal pregnancy decreases from when a woman is in her early 30s into her 40s. A woman is rarely fertile beyond the age of 45. This applies to the ability to conceive with her eggs, but not with donor eggs.
2) Ovulation disorders
Normal and regular ovulation, or release of a mature egg, is essential for women to conceive naturally. Ovulation often can be detected by keeping a menstrual calendar or using an ovulation predictor kit. There are many disorders that may impact the ability for a woman to ovulate normally. The most common disorders impacting ovulation include polycystic ovary syndrome (PCOS), hypogonadotropic hypogonadism (from signaling problems in the brain), and ovarian insufficiency (from problems of the ovary). If your cycles are infrequent or irregular, your doctor will examine you and perform the appropriate testing to discover which problem you may have and present the appropriate treatment options.
3) Tubal occlusion (blockage)
As discussed previously, a history of sexually transmitted infections including chlamydia, gonorrhea, or pelvic inflammatory disease can predispose a woman to having blocked fallopian tubes. Tubal occlusion is a cause of infertility because an ovulated egg is unable to be fertilized by sperm or to reach the endometrial cavity. If both tubes are blocked, then in vitro fertilization (IVF) is required. If a tube is blocked and filled with fluid (called a hydrosalpinx), then minimally invasive surgery (laparoscopy or hysteroscopy) to either remove the tube or block/separate it from the uterus prior to any fertility treatments is recommended.
4) Uterine fibroids
Fibroids are very common (approximately 40% of women may have them) and the mere presence alone does not necessarily cause infertility. There are three types of fibroids: 1) subserosal, or fibroids that extend more than 50% outside of the uterus; 2) intramural, where the majority of the fibroid is within the muscle of the uterus without any indentation of the uterine cavity; and 3) submucosal, or fibroids the project into the uterine cavity. Submucosal fibroids are the type if fibroid that has clearly been demonstrated to reduce pregnancy rate, roughly by 50%, and removal of which will double pregnancy rate. In some cases, simply removing the submucosal fibroid solves infertility. Often, but not always, submucosal fibroids can cause heavy periods, or bleeding between periods. There is more controversy regarding intramural fibroids, where larger ones may have an impact and may necessitate removal. Subserosal fibroids do not affect pregnancy. Your physician will examine you carefully to determine if you have fibroids and if removal is necessary.
5) Endometrial polyps:
Endometrial polyps are finger-like growths in the uterine cavity arising from the lining of the uterus, called the endometrium, These abnormalities are rarely associated with cancer (<1% in a woman before menopause), but polyps are can decrease fertility by up to 50% according to some studies. Removal of polyps by the minimally invasive procedure hysteroscopy is associated with a doubling of pregnancy rate. In some cases, simply removing the polyp solves infertility.
6) Male factors affecting sperm function
Male factor infertility has been associated as a contributing factor causing infertility in 40-50% percent of cases, and as the sole cause for infertility in 15-20% percent of cases. If a semen analysis is found to be abnormal, generally it is first repeated to confirm the abnormality. Once confirmed, the male partner is referred to a reproductive urologist, especially if the abnormality is severe. In some cases, the reproductive urologist can improve semen function by recommending certain lifestyle changes, by hormonal treatments, or by surgery. In most cases however, sperm function may not improve and therefore any attempts at pregnancy may require additional treatments or procedures performed by our clinic. Options include intrauterine insemination (also known as IUI) or IVF with intracytoplasmic sperm injection (also known as ICSI).
- Intrauterine insemination is a process by which sperm is washed and prepared for placement into the uterine cavity, therefore bypassing the cervix and bringing a higher concentration of motile sperm closer to the tubes and ovulated egg. At least one open tube is required for IUI, and the sperm abnormality cannot be severe otherwise the sperm will not be able to swim to and fertilize the egg.
- Intracytoplasmic sperm injection is a process by which semen is washed and prepared for direct injection of one sperm into each egg collected during the IVF process. In order to perform ICSI, an egg is held via a small suction pipette, while one sperm is injected into that egg using a very fine glass needle. This process bypasses the normal fertilization process, which may be compromised due to poor sperm function. Your doctor will analyze your semen analysis carefully and help you decide if ICSI is an appropriate treatment for you.
7) Endometriosis
Endometriosis is a condition whereby cells very similar to the ones lining the uterine cavity, or endometrium, are found outside the uterine cavity. It is found in approximately 10-50% of reproductive-aged women and can be associated with infertility as well as pain during intercourse and/or menstrual periods. Endometriosis causes infertility by producing inflammation and scarring, which can result in not only pain but also potentially detrimental effects on egg, sperm or embryo. Endometriosis can only be confirmed by surgery, usually laparoscopy. If endometriosis is found, it can be surgically removed by various methods, and its removal may lead to a decrease in pain as well as improvement in the ability to conceive naturally. Your doctor will determine if you are at risk of having endometriosis based on a careful history, physical exam, and ultrasound.
8) Unexplained/other
Sometimes a full evaluation does not reveal the cause of infertility. This occurs approximately 15% of the time. Thankfully, even when the cause of infertility is not known, various fertility treatments can overcome the unknown road block that was preventing pregnancy and eventually lead to delivery of a healthy baby.
What are the Treatment Options?
Treatment for Infertility
1) Education
We strongly believe that educating our patients about the normal process of fertility, problems that affect fertility, and treatment options will empower our patients to make the best choices. Understanding the normal reproductive process is essential in knowing when to seek help. Helping our patients develop a deep understanding of their fertility options will make the process smoother. Our goal is to have each and every patient feel as part of our team, a team that is focused on helping them have a healthy baby. For those interested, we offer a free class entitled, “The Couple’s Guide to IVF”, that meets twice monthly and is open to the public.
2) Medications to induce egg development and ovulation
The medications that help stimulate the ovary to develop mature eggs for ovulation come in two forms: pills taken by mouth and injections. The most commonly prescribed pill to stimulate ovulation (generally of one mature egg) is clomiphene citrate. This pill generally is taken from menstrual cycle days 3 – 7. It works in the following way: Clomiphene is an anti-estrogen. It binds in a part of the brain called the hypothalamus, which is essential in stimulating the ovary to grow and release an egg. When clomiphene binds to estrogen receptors in the hypothalamus, it leads to an increase release of an important signaling hormone called GnRH (gonadotropin releasing hormone). This hormone then binds to another area of the brain called the pituitary gland and leads to the release of FSH (follicle stimulating hormone), a hormone that directly binds to cells in the ovary, leading to egg growth and maturation.
The most commonly prescribed injections that stimulate the ovary are called gonadotropins. The gonadotropins in these formulations are FSH, and in some cases, a combination of FSH and LH (luteinizing hormone). These injections are taken nightly, typically for 5 – 10 days, and act directly on the cells of the ovary to stimulate egg development. Once a follicle containing an egg reaches a mature size, another hormone injection called HCG is often given to mimic the natural LH surge that occurs at the time of ovulation. This leads to the final maturation and release of the egg.
3) Insemination
Intrauterine insemination, also known as IUI, is a process by which sperm is washed and prepared for placement into the uterine cavity, therefore bypassing the cervix and bringing a higher concentration of motile sperm closer to the tubes and ovulated egg. In order to accomplish this, the semen is washed with a solution safe to sperm and eggs, and then centrifuged to separate motile sperm from immotile sperm and other cells. Those motile and viable sperm are then placed in a very small amount of solution, and then very gently and painlessly injected into the uterine cavity using a very thin, soft, and flexible catheter. At least one open tube is required for IUI, and any sperm abnormality cannot be severe, otherwise the sperm will not be able to swim to and fertilize the egg.
4) In Vitro Fertilization (IVF)
In vitro means “outside the body.” IVF is a process whereby eggs are collected and then fertilized by sperm outside the body, in an embryology laboratory. The first IVF baby was born in 1978 in England. Not long after, the United States delivered its first IVF baby, and the use of IVF has grown dramatically. IVF was a major breakthrough because it allowed for successful pregnancies in women that were previous deemed permanently infertile, such as when the fallopian tubes are both markedly damaged. IVF involves removal of eggs directly from the ovary, fertilization with sperm in the laboratory, followed by transfer of the embryos directly into the uterus, thereby bypassing the tubes. Although tubal disease was the original indication for IVF, many more indications have developed over the years. These include advancing maternal age, severe male factor infertility (whereby ICSI can be used to fertilize the egg), and endometriosis, amongst many others.
IVF is generally performed in the following manner:
- The woman undergoes gonadotropin injections, which stimulate the ovaries to produce many eggs. Once the follicles (fluid filled sacs containing the eggs) reach a mature size, an HCG injection is administered which leads to final development and maturation of the eggs. Just before those eggs would otherwise be ovulated, they are retrieved under mild anesthesia in an operating room. This procedure is done by ultrasound guidance when the surgeon utilizes a narrow needle to retrieve eggs from the ovary through the vaginal wall. This sterile needle is attached to sterile suction tubing and a collecting vial. Once the fluid containing the eggs is removed from the follicles into the vials, they are handed to the embryologist who finds the eggs, places them in tiny droplets on a Petri dish, and then fertilizes the eggs using their partner’s or donor sperm. The sperm can either be mixed with the eggs to allow normal fertilization (conventional insemination) or by injecting one sperm into each mature egg (ICSI).
- The fertilized eggs, now embryos, are allowed to grow and develop in culture media for typically 3 to 5 days. Then, generally one or two embryos, which have demonstrated appropriate development, are carefully and gently transferred into the uterine cavity. Embryos transfer is performed in the office under abdominal ultrasound guidance using a small, soft, sterile and flexible catheter. The embryos are placed within the tip of the transfer catheter and then injected within the uterine cavity once the catheter is placed through the cervical canal to the ideal spot within the uterus.
- The pregnancy test is then performed 2 weeks after the egg retrieval. This process has revolutionized assisted reproductive technology and the way reproductive endocrinologists can help people in having a baby. Free IVF Class | Class Testimonials
5) Third party reproduction
This is a general reference to a general process where another person provides sperm or eggs, or where another woman acts as a gestational surrogate, with the purpose of helping another person or couple have a child. The four types of third party reproduction are 1) sperm donation – a process by which donated sperm is used for insemination in the uterus, or for fertilization of eggs in the IVF process; 2) egg or ovum donation – a process by which an egg donor undergoes an IVF cycle in order to obtain her eggs which are then donated and fertilized. The resulting embryos are then transferred into the uterus of the future mother, known as the recipient. Usually no more than 1 – 2 embryos are transferred, and therefore additional embryos can be frozen, or cryopreserved, for future use; 3) embryo donation – a process where a fully developed embryo from another person in combination w/donor sperm, or couple who underwent IVF, are donated to another woman, the future intended mother, for transfer into her uterus; and 4) gestational surrogacy – a process where another woman will undergo an embryo transfer and carry the pregnancy for another person. Your physician will discuss these approaches to having a baby if appropriate to your particular case.
6) Surgery
After a thorough history, physical examination, and ultrasound are performed, your doctor may recommend surgery to correct and abnormality. In reproductive medicine, the most common surgical procedures are laparoscopy, hysteroscopy, and abdominal myomectomy (removal of uterine fibroids).
Laparoscopy is an operation performed in the abdomen or pelvis through small incisions, generally no more than a centimeter, with the assistance of a laparoscope attached to a camera which projects to a screen. It can either be used to inspect and diagnose certain conditions or to surgically correct an abnormality such as removing scar tissue, endometriosis, or a damaged fallopian tube. The procedure is performed in an outpatient setting in the vast majority of cases, and recovery time can be as little as a few days.
Hysteroscopy is the inspection of the uterine cavity through the cervix by a hysteroscope attached to a camera which projects to a screen. Through this technique, your physician can diagnose abnormalities such as fibroids or polyps within the uterine cavity, and via narrow instruments that run through the hysterosope, can remove or correct the great majority of these abnormalities. This procedure is performed in the outpatient setting. Recovery is generally no more than one day. Hysteroscopy can also be combined with laparoscopy when necessary.
Abdominal myomectomy is a surgical procedure performed through a very low horizontal abdominal incision allowing access to the uterus for removal of fibroids. This procedure can, in selected cases, also be performed laparoscopically, often with the assistance of a robot.