High Calcium Levels & Primary Hyperparathyroidism
Find your care
We deliver effective, minimally invasive treatments in a caring environment. Call 310-267-7838 to connect with an expert in endocrine surgery.
Parathyroid Disease & Hypercalcemia
At UCLA Endocrine Center, we specialize in the treatment of parathyroid diseases. We take care of patients who have been newly diagnosed with elevated blood calcium as well as patients who have persistent disease despite previous surgery. If you are seeking help for persistent disease after previous surgery, learn about reoperations for primary hyperparathyroidism.
What is Hypercalcemia (High Blood Calcium)?
When your doctor orders routine blood tests, it is common to check a blood calcium level. The finding of a high blood calcium level is very common, occurring in millions of Americans each year. Sometimes, this will just be a single event related to a laboratory error or being dehydrated on the day the lab was drawn. The first thing to do is to recheck the value with another blood test. When you have two or more blood tests showing high levels of calcium in your blood, we consider that hypercalcemia, and encourage
Learn more about calcium levels.
Causes of High Calcium
UCLA endocrine surgeons Masha Livhits, MD & Michael Yeh, MD, presented a live-streaming webinar to discuss what causes hypercalcimia, or high levels of calcium in your blood which can weaken your bones, create kidney stones and interfere with how your heart and brain work.
What Causes Hypercalcemia?
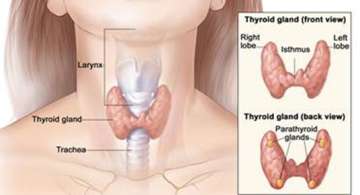
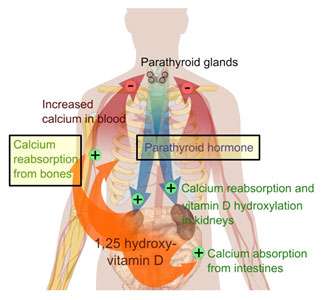
Primary hyperparathyroidism is the most common cause of high blood calcium level in the general population. Primary hyperparathyroidism is when your parathyroid glands make excessive amounts of parathyroid hormone (PTH). Parathyroid hormone tells your bones, intestines, and kidneys to raise the level of calcium in your blood. The disease is most common in people over 60 but can also be seen in younger adults. Women are more likely to be affected than men. Other causes of high blood calcium include:
- Taking too much calcium supplements, vitamin D, or vitamin A
- Certain medications, such as Hydrochlorothiazide (HCTZ) or Lithium
- Alcohol abuse
- Other rare causes not listed here
How is Primary Hyperparathyroidism Diagnosed?
Initial evaluation of hypercalcemia begins with:
- Assessment by endocrinologist or endocrine surgeon
- Review of your blood tests, focusing on calcium and parathyroid hormone (PTH)
The diagnosis of primary hyperparathyroidism can be made on laboratory tests alone and does not require any imaging studies. The most classic pattern is to have an elevated blood calcium levels as well as a high level of parathyroid hormone. However, a significant proportion of patients with primary hyperparathyroidism can have parathyroid hormone levels in the “normal” range. In those cases, we often will also perform additional blood tests and even urine tests to help confirm the diagnosis.
What if I have elevated parathyroid hormone (PTH) but normal calcium?
Normal calcium levels despite high blood levels of parathyroid hormone could be a result of:
- Vitamin D deficiency
- Very low amounts of dietary calcium over a long period of time
- Intestinal diseases that interfere with absorption of calcium (e.g. celiac disease)
- Normocalcemic hyperparathyroidism
Normocalcemic hyperparathyroidism is a rare disease. Similar to primary hyperparathyroidism, the parathyroid glands are making too much hormone. However, in this disease, the calcium does not rise to an abnormal level. These are challenging diagnoses, and treatment plans should be tailored to each individual patient. Thus, we recommend consultation with our endocrinologists and endocrine surgeons. More about normocalcemic hyperparathyroidism.
What are the Signs and Symptoms of Primary Hyperparathyroidism?

The signs and symptoms of primary hyperparathyroidism come from a combination of the effect of excess parathyroid hormone and high levels of calcium on different organs:
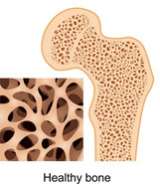
Osteopenia, osteoporosis, or fractures – caused by abnormal removal of calcium from bones, can also cause bony pain / muscle pain
Kidney stones – the kidneys filter the calcium from the blood into the urine, but the high amount of calcium can crystallize into kidney stones, which can cause flank pain and bloody urine

Impaired kidney function – the extra calcium can form deposits in the kidney, lowering kidney function slowly over time
Increased urination and thirst – filtering the extra calcium also filters water, leading to frequent urination with dehydration and thirst
Vague abdominal pain, constipation, nausea, loss of appetite – high levels of calcium also affects the GI tract, in rare cases patients can also develop pancreatitis
Changes in mood or concentration, depression, fatigue – related to calcium’s affect on the nervous system, but this is less well understood
How Is Primary Hyperparathyroidism Treated?

The treatment options for primary hyperparathyroidism are:
- Surgical removal of abnormal parathyroid gland(s) (parathyroidectomy)
- Medications to reduce bone loss and/or reduce blood calcium level
- Observation / monitoring
Treatment depends on age and how severe your symptoms are. Surgery is typically recommended for:
- Patients with osteoporosis or fractures caused by low bone mineral density
- Patients with kidney stones or impaired kidney function
- All patients younger than 50 years of age, since future problems are likely to manifest in the patient’s lifetime
If surgery is the best treatment option for you, the next step is to determine which of the four parathyroid glands may be enlarged and making the excess hormone.
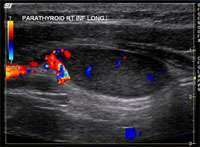
Most commonly, one of the four parathyroid glands have enlarged. However, it is possible to have two enlarged glands, or even mild growth of all 4 glands. Proper imaging tests help create a roadmap for a successful surgery. We routinely obtain multiple tests. Imaging of the parathyroid glands is challenging and sometimes the abnormal gland is not definitively seen by one or more imaging tests. That is because a normal parathyroid gland is the size of a grain of rice, and an abnormal gland may be the size of a green pea. Imaging is usually a combination of the following:
- Neck ultrasound, performed by the endocrine surgeon during the office visit
- Parathyroid 4D CT scan
- Sestamibi scan or SPECT (single proton emission computerized tomography) scan

What is a parathyroid 4D CT scan?
Parathyroid 4D-CT represents the latest technology in parathyroid imaging. The resolution of 4D-CT imaging is higher than that of any other type of parathyroid scan. Parathyroid 4D-CT is particularly useful when other imaging studies have been negative (failed to show the abnormal parathyroid gland) or when the anatomy of the neck has been distorted by prior surgery or co-existent thyroid disease. In our experience at UCLA of reading several hundred scans per year, we have been able to detect at least one abnormal parathyroid gland in 99% of cases. In other words, parathyroid 4D-CT is a highly sensitive scan.
A parathyroid 4D-CT needs to be performed at an experienced, high-volume center. we have spent considerable effort optimizing 4D-CT for our patients with challenging parathyroid disease. This process of continuous quality improvement took several years: one year to optimize the scanning technique (2011), another year to validate the results in comparison to actual surgical findings in a standard patient population (2012), and a third year (2013) to validate the results in a more challenging patient population (principally patients who had had failed parathyroid surgery elsewhere who came to us for re-do surgery). More information on parathyroid 4D CT.

What Are the Benefits of Parathyroid Surgery?
Certain benefits are clearly established, and others less so. This is because primary hyperparathyroidism can cause a wide constellation of symptoms, many of which can be vague or nonspecific. There are certain symptoms that reliably improve with surgery because we are certain they are caused by primary hyperparathyroidism. Here is what to expect.
View an in-depth review of the medical literature behind this advice.
Bone Health Will Improve
Improvements in bone mineral density following parathyroid surgery are very well established, and patients can routinely expect these benefits soon after surgery. Bone mineral density will significantly increase in the year following surgery, and continue to increase over the next 10 years.
Bone Health and Hyperparathyroidism
UCLA endocrine surgeons Michael Yeh, MD, and Masha Livhits, MD, discuss hyperparathyroidism (overactive parathyroid glands), the role of parathyroid glands in regulating calcium levels, and treatments that can help maintain bone health.
Updates for Hyperparathyroidism and Osteoporosis
UCLA endocrine surgeons Masha Livhits, MD, and Michael Yeh, MD, discuss the latest research and treatment options for hyperparathyroidism and osteoporosis.
Risk of Kidney Stones Will Decrease
Patients who undergo surgery drastically reduce the chances of having a future kidney stone. However, it takes approximately one year after surgery for the risk to fall.
Overall Quality of Life Will Improve
It is now well known that patients with primary hyperparathyroidism report an overall improvement in their quality of life after surgery. This is related to an improvement in a number of areas: fatigue, exhaustion, pain in the muscles and bones, weakness, frequent urination, constipation, depression, and others. Sometimes these symptoms have come on so slowly that patients do not recognize they have been affected until after they improve. These following symptoms may also improve after parathyroid surgery in some patients, but not all, after parathyroid surgery.
- Improvement in vague abdominal pain, constipation, nausea
- Improvement in mood, concentration, or depression
- Very modest improvement in blood pressure
- Possible reduction in risk of cardiovascular events
Bone mineral density improves after parathyroid surgery. Patients having surgery are shown in teal, patients not having surgery are shown in burgundy. Figures show changes in bone density at 1, 4, 7, and 10 years after surgery. Parathyroid surgery leads to prompt increases in bone density in both the spine and hip. These improvements continue for 10 years after surgery. (Adapted from Silverberg, NEJM 1999) View larger image.
Reduction in kidney stone events after parathyroid surgery. Immediately prior to surgery, the risk of stone events is approximately 400 times normal. That risk rapidly declines during the first year following surgery, though a return to completely normal risk levels takes several additional years. (Adapted from Mollerup, BMJ 2002). Larger image.
Symptoms improve after parathyroid surgery. After surgery, individuals with primary hyperparathyroidism (shown in burgundy) experience a marked decrease in the symptoms listed above when compared to individuals without parathyroid disease, who underwent a thyroid operation (shown in teal). Overall, approximately 70% of patients who undergo parathyroid surgery experience improvement in one or more of their symptoms. Equivalent rates of improvement are seen for patients with biochemically mild disease (those not meeting NIH criteria for surgery) and those with biochemically severe disease (those meeting NIH criteria for surgery). (Adapted from Chan, Ann Surg 1995; and Eigelberger Ann Surg 2004) Larger image

How is Parathyroid Surgery Performed?
Watch video of parathyroid surgery.
This describes our main technique for minimally invasive parathyroidectomy with a 4 gland exploration through a central mini-incision, though variations exist. We begin with a 1-inch skin incision, hidden in a skin crease if possible.
What surgical technique is used and why?

We use either a focused lateral mini-incision technique or a central mini-incision technique. An incision length of approximately 2.0 cm (about ¾ inch) is used regardless of the approach and regardless of how many parathyroid glands are examined. Sometimes, in large or obese people, the incision is slightly longer. The operation is done under direct vision, without the use of a videoendoscope. In our opinion, this technique provides direct access to the parathyroid glands, minimizes tissue injury, and has superior cosmetic results.
Indeed, every surgeon will have his or her own technique of performing parathyroid surgery. And that doesn’t matter. Experience does. So please do not let anyone convince you that their specific method is somehow superior. In most cases we believe it is beneficial to inspect more than 1 parathyroid gland, and often we inspect all 4. But of course this depends on the individual patient.

How Long is Parathyroid Surgery?
The average operating time is under 1 hour, with many operations being completed in less than 30 minutes. Though we value efficiency, we do not necessarily equate fast surgery with good surgery. Patient safety is our utmost priority. Ultimately, our operations take as long as necessary to complete in a safe and meticulous manner. We are here to take excellent care of each patient, one patient at a time. If one of us were to have surgery we would not want it to be rushed. So we are not going to rush your surgery.
What is the Appearance of the Scar After Parathyroidectomy?
All other things being equal, a small incision is nice to have. The reason we put incision size somewhat lower down on this priority list is that, at present, there is really not much difference in the incision sizes offered by expert parathyroid surgeons. They are all around 1 inch (2.5 cm). We do pay attention to incision length and cosmetic appearance because the neck is a difficult part of the body to cover up, and a significant number of our patients make a living on camera (see our Scar gallery).
Intra-operative Parathyroid Hormone (IOPTH) Monitoring

To maximize success rates of parathyroid surgery and prevent disease from coming back, we monitor parathyroid hormone levels in real time during the operation. This is known as intra-operative parathyroid hormone monitoring (IOPTH). We utilize the very latest rapid IOPTH assay platform, which returns results within 8 minutes. An adequate decrease in parathyroid hormone level gives us confirmation that surgery has been successful.
What Should I Expect After Surgery?
Patients are observed for a few hours after surgery, then most patients return home the same day. The observation period allows us to ensure your pain control is adequate, check your calcium levels after surgery, and watch for any signs of hematoma. We do recommend that patients who live far away from the hospital stay overnight and return home the next day. Patients are able to return to normal light activities right away. We advise that strenuous activities, such as heavy lifting or sports, be avoided for 5 days after surgery. Most patients are physically able to return to work the day after surgery, though most choose to take a few days off to recover at their own pace. We do ask that patients refrain from driving until they are no longer taking narcotic pain medication and can comfortably move their head from side to side. Most patients report adequate pain control on Tylenol alone.
What to Expect After Parathyroid Surgery
UCLA endocrine surgeons Masha Livhits, MD, and Michael Yeh, MD, talk about short- and long-term expectations after parathyroid surgery.
Frequently Asked Questions (FAQs)

What is Secondary Hyperparathyroidism?
Secondary hyperparathyroidism usually occurs in patients with kidney failure (dialysis patients). The body is unable to clear phosphorous and make enough Vitamin D, which causes low blood levels of calcium. This stimulates the parathyroid glands to grow and produce extra parathyroid hormone. Secondary hyperparathyroidism is usually treated with medications such as cinacalcet (Sensipar), and surgery is reserved for cases where the medications fail to work. If the kidney failure resolves (usually after a kidney transplant), secondary hyperparathyroidism usually resolves as well. If hyperparathyroidism does not resolve after a kidney transplant, this is called tertiary hyperparathyroidism and surgery may be necessary (usually subtotal parathyroidectomy, which is removal of three and a half parathyroid glands). More about secondary hyperparathyroidism.
What is Osteoporosis?
Osteoporosis is a weakening of your bones, which increases the risk of a fracture. People with osteoporosis have bones that break too easily (for example, after a fall on the sidewalk).
What Conditions Can Cause Osteoporosis?
Osteoporosis is most common in post-menopausal women. Additional causes of osteoporosis should be considered especially in younger (pre-menopausal) women and men. These include:
- Hyperparathyroidism
- Hyperthyroidism
- Testosterone deficiency (in men)
- Estrogen deficiency (in women)
- Gastrointestinal disease causing malabsorption (such as celiac disease)
- Calcium or vitamin D deficiency
- Cushing’s syndrome
- Kidney or liver disease
- Smoking or excessive alcohol intake
- Sedentary lifestyle or inability to exercise (especially with neuromuscular conditions or paralysis)
- Medications: steroids, proton pump inhibitors (used for heartburn), heparin (used to prevent or treat blood clots), aromatase inhibitors such as Arimidex or Femara (used to prevent estrogen production in breast cancer treatment), phenytoin (used to treat seizure disorders)
Does Osteoporosis Cause Bone Pain or Achy Joints?
It is a common misconception that osteoporosis usually causes bone pain. In fact, most people have no symptoms unless there is a fracture. So a person can be completely free of pain and still have osteoporosis. Vertebral fractures (in the spine) can also be painless but cause progressive loss of height over time.
I Eat a Diet That is High in Calcium. Why Did I Still Get Osteoporosis?
Answer: Calcium is only one component of keeping your bones healthy. There are other risk factors for osteoporosis including genetics (having a family member with osteoporosis), the conditions listed above, and aging (especially for women).
How Does Hyperparathyroidism Cause Osteoporosis?
Answer: Hyperparathyroidism causes one or more of the parathyroid glands to produce too much parathyroid hormone (PTH). PTH increases bone turnover, and too much PTH causes cortical bone thinning especially in the femoral neck (thigh) and distal radius (forearm).
How is Osteoporosis Detected?
The main way to diagnose osteoporosis is with a bone density scan called dual-energy x-ray absorptiometry (DXA). X-ray beams are aimed at the patient’s bones, allowing the bone density to be measured at multiple areas including the spine, hip, and forearm. Patients with osteoporosis have a T-score of less than 2.5, which is a comparison between the patient’s bone density and the average bone density of a young adult.
Are There any Blood Tests That Can Detect Osteoporosis?
Bone turnover markers have been developed that can be checked with a blood test. These include osteocalcin, bone alkaline phosphatase, and Type 1 collage peptides (NTX and CTX). Their role in the clinical care of patients is still being investigated. Bone turnover markers often improve following parathyroidectomy. Currently there are no specific recommendations for routinely checking bone turnover markers before or after parathyroidectomy.
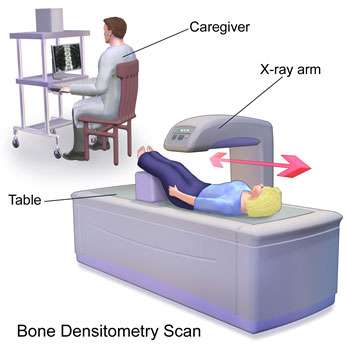
Should All Patients With Hyperparathyroidism Have a Bone Density Scan?
Answer: According to the 2016 American Association of Endocrine Surgeons (AAES) Guidelines, the answer is yes. Patients with hyperparathyroidism should have a DXA scan to check bone mineral density at the lumbar spine, hip, and distal radius. A repeat DXA scan may be recommended 1 year following parathyroidectomy to look for changes in the bone density.
How Can Patients With Hyperparathyroidism Minimize Bone Loss While Waiting for Parathyroidectomy?
The best way to keep your bones healthy is with weight-bearing exercise, if possible 30 minutes daily at least 4 times per week. This does not mean you have to lift weights. These are exercises that you do while on your feet so that your bones have to work against gravity to support you. Of course, be careful not to fall especially if you have problems with balance.
Some examples include:

- Brisk walking or jogging (outside or on a treadmill)
- Hiking
- Dancing
- Step aerobics
- Stair climbing
- Tennis or other sports involving a racquet or ball
- Yard work like heavy gardening
Vitamin D supplementation can help in patients with Vitamin D deficiency. You should also avoid smoking and excessive alcohol use.