Breast MRI Findings: Breast Implant
by Emeka Okafor, MD, Fadi Dahoud, and Laura Doepke, MD
Background
Women living with breast implants in the United States is becoming exceedingly common today. Based on available data, approximately 4% of all women in the United States currently have breast implants1. The prevalence of women with breast implants is expected to grow as the popularity ofcosmetic breast augmentation and the need for breast reconstruction procedures continueto rise. According to the American Society of Plastic Surgeons, breast augmentation remains as one of the top 5 cosmetic surgical procedures for the past 14 years whereas breast reconstruction is one of the top reconstructive procedures performed annually2.
With the increase of breast implants in the general population, optimal imaging techniques for breast prosthesis are at theforefront of breast radiology.Magnetic resonance imaging (MRI) is largely regarded as the gold standard for imaging implant-augmented breasts demonstrating high sensitivity and specificity in detecting implant-related abnormalities.The advantages of MRI are based on its ability to delineate between water, fat, muscle, and silicone material while maintaining high spatial and soft tissue resolution3.
Implant Material
There are two types of breast prosthetic material approved for use in the United States by the Food and Drug Administration (FDA) which include saline and silicone gel implants. Saline implants are filled with isotonic sterile salt water. Although considered less natural in appearance, saline is physiologically absorbed by the body in the setting of leak/rupture without major complications4, 5. Saline implants, unlike silicone, will have a valve along its outer surface which is apparent on MRI. Silicone gel implants are inflated with a highly viscous silicone substance that better mimics the firmness, texture, and profile of natural breast tissue (Figure 1). Silicone implants are the most common material type constituting 84% of implants used by surgeons in 2020 alone compared to only 16% of saline implants. Rarer implant materials include polyurethane, sponges, and polypropylene6, 7.
Implant Lumen
In addition to the material type, breast implants can be further characterized by lumen number. Regardless of the material, all implants are constructed with a multilayer silicone-based outer shell. A single-lumen implant is entirely filled with either saline solution or silicone gel. A double-lumen implant is composed of two separate compartments8. A standard double-lumen implant incorporates a saline-filled outer lumen with a larger silicone-filled inner lumen. An inverse double-lumen implant has a silicone-filled outer lumen and an expandable saline-filled inner lumen. Once placed, an expected inflammatory response produces a fibrous scar which encapsulates the outer shell of the implant9.
Implant Location
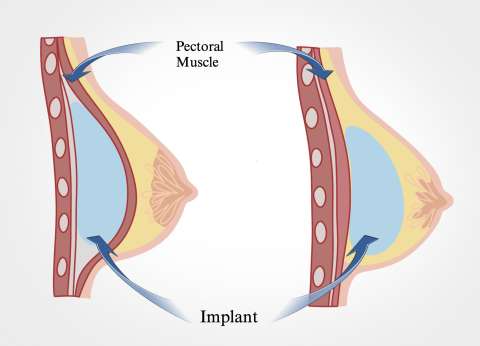
Breast Implants are surgically positioned in relation to the glandular breast tissue and pectoralis major musculature. Retroglandular implants are placed under the glandular tissue but above the pectoralis major. In contrast, retropectoral implants are placed deep to the pectoralis major muscle (Figure 2). Precise knowledge of the implant location can aid with identification of herniation and help interpret contour deformities4.
MRI Implant Imaging Techniques
MRI techniques for implant imaging incorporate several sequences that rely on the difference in intensities between water and silicone. The most common sequences include T2-weighted, short-time inversion recovery silicone-sensitive (silicone hyperintense, water hypointense), and silicone-saturated (silicone hypointense, water hyperintense) images3, 6. Although contrast enhanced sequences are useful for evaluating disease processes such as neoplasms in an implant-augmented breast, they are not necessary for the imaging of breast prosthesis10.
Implant Rupture
A primary role of MRI implant imaging entails the evaluation of implant integrity. The risk of implant rupture increases with the age of the implant, most commonly occurring 10-15 years postplacement. While the cause of rupture in most cases are attributed to natural aging of the implant beyond its indicated lifespan, other etiologies include manufacturing defects and trauma11. Implant rupture can clinically present with loss of normal implant contour, implant displacement, and/or pain. Ruptures can be categorized as intracapsular or extracapsular based on the location of extravasated implant material in relation to the fibrous capsule. For intracapsular rupture, the implant material extrudes through theouter shell of the implant while the fibrous capsule remains intact12, 14. Extracapsular rupture involves the extravasation of implant material outside of the fibrous capsule. Implant ruptures can also be classified by degree of implant shell collapse ranging from uncollapsed to fully collapsed. MRI findings of implant rupture depend on a combination of the aforementioned categories13.
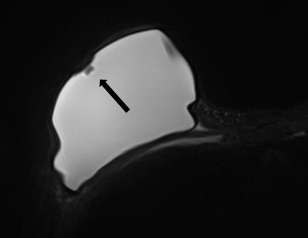
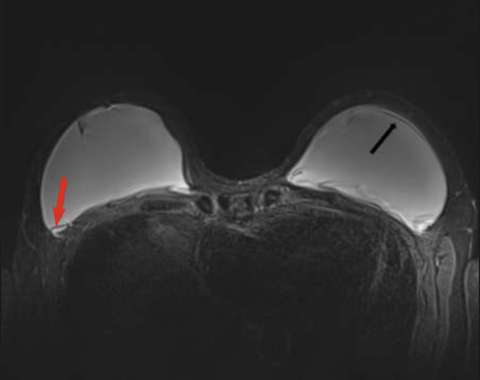
Minimally collapsed intracapsular rupture appears as a hypointense line that runs parallel to the fibrous capsule against the hyperintense extravasated silicone gelon silicone-sensitive MRI images, termed the “subcapsular line sign” (Figure 3).
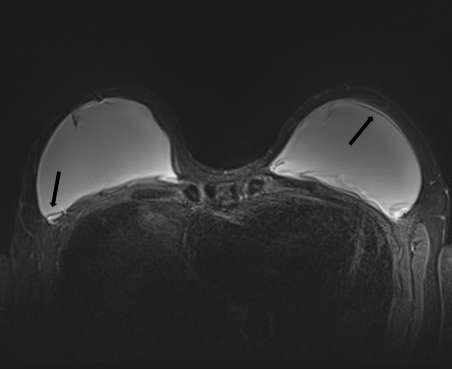
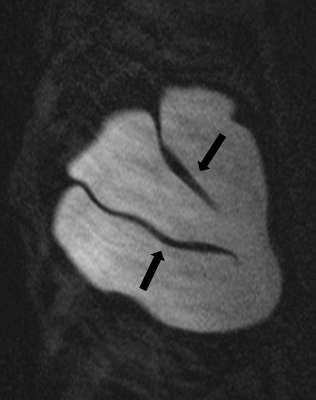
Fully collapsed intracapsular ruptures appear as multiple hypointense curvilinear lines that float within the hyperintense silicone gel, referred to as the “linguine sign” (Figure 4). The floating curvilinear lines represent the collapsed outer shell6.

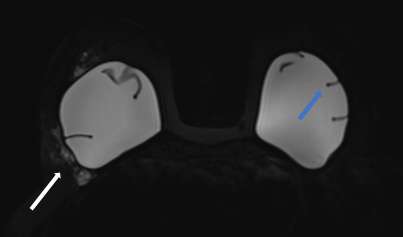
Intracapsular rupture with focal collapse of the outer shell will result in the “keyhole sign”, also referred to as the “noose sign”. This sign appears as a focal invagination of the hypointense outer shell where the two membranes do not touch. Similarly, the “teardrop sign” appears as a focal invagination of the hypointense outer shell containing a droplet of hyperintense extravasated silicone gel with the partial apposition of the two membranes13 (Figure 5).
Extracapsular ruptures appear as free silicone material extending beyond the fibrous capsule into the adjacent tissues on T2-weighted and silicone-sensitive sequences3 (Figure 6).
Radial Fold
Radial folds are normal invaginations of the outer shell and can mimic intracapsular ruptures. They are seen as hypointense lines that extend from the periphery and are perpendicular in orientation to the implant capsule (Figure 7). Radial folds can appear as simple or complex folding patterns but are continuous when traced in different imaging planes. Considered a normal variant, radial folds are most commonly caused by capsular contracture9.
Focal Bulge
A focal bulgeis due to a focal breakdown of the fibrous capsule which allows for protrusions of the underlying implant. On MRI, the protrusions appear as contour deformity along an intact outer shell. A focal bulge is associated with an increased risk of implant rupture due to the weaking of the adjacent capsule15.
Silicone-Filled Lymph Nodes
Leakage of free silicone with distant translocation can manifest as silicone lymphadenopathy through significant extracapsular implant rupture, or a process known as “gel bleed.” Gel bleed is characterized by microscopic release of silicone due to molecular breakdown of the outer shell caused by differences in chemical bonding between the composite materials found in older generation implants. Free silicone droplets are transported to the regional lymph nodes and appear as enlarged isointense nodes on MRI16, 17, 18.
References:
- Voltz D. How Many Women Have Breast Implants? Modern Plastic Surgeon. 2014 [cited 2021 Dec 9]
- Plastic Surgery Statistics. American Society of Plastic Surgeons. [cited 2021 Dec 1].
- Wong T, Lo LW, Fung PY, Lai HY, She HL, Ng WK, Kwok KM, Lee CM. Magnetic resonance imaging of breast augmentation: a pictorial review. Insights Imaging. 2016 Jun;7(3):399-410. DOI: 10.1007/s13244-016-0482-9.
- Wiedenhoefer J, Shahid H, Dornbluth C, Otto P, Kist K. MR imaging of breast implants: Useful information for the interpreting radiologist. [cited 2021 Dec 1.]
- Breast Implants - Certain Labeling Recommendations to Improve Patient Communication - Guidance for Industry and Food and Drug Administration Staff. :22.
- Juanpere S, Perez E, Huc O, Motos N, Pont J, Pedraza S., Imaging of breast implants—a pictorial review. Insights Imaging. 2011 Dec;2(6):653-670. DOI: 10.1007/s13244-011-0122-3.
- Green LA, Karow JA, Toman JE, Lostumbo A, Xie K., Review of breast augmentation and reconstruction for the radiologist with emphasis on MRI. Clin Imaging. 2018 Jan-Feb;47:101-117. DOI: 10.1016/j.clinimag.2017.08.007.
- Berg WA, Anderson ND, Zerhouni EA, Chang BW, Kuhlman JE., MR imaging of the breast in patients with silicone breast implants: normal postoperative variants and diagnostic pitfalls. AJR Am J Roentgenol. 1994 Sep;163(3):575-8. DOI: 10.2214/ajr.163.3.8079848.
- Shah M, Tanna N, Margolies L., Magnetic resonance imaging of breast implants. Top Magn Reson Imaging. 2014 Dec;23(6):345-53. DOI: 10.1097/RMR.0000000000000039.
- Kim SH, Lipson JA, Moran CJ, Shimakawa A, Kuo J, Ikeda DM, Daniel BL., Image quality and diagnostic performance of silicone-specific breast MRI. Magn Reson Imaging. 2013 Nov;31(9):1472-8. DOI: 10.1016/j.mri.2013.05.011.
- Swezey E, Shikhman R, Moufarrege R. Breast Implant Rupture. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Bookshelf ID: NBK459308
- Seiler SJ, Sharma PB, Hayes JC, Ganti R, Mootz AR, Eads ED, Teotia SS, Evans WP., Multimodality Imaging-based Evaluation of Single-Lumen Silicone Breast Implants for Rupture. Radiographics. 2017 Mar-Apr;37(2):366-382. DOI: 10.1148/rg.2017160086.
- Yang N, Muradali D.,The augmented breast: a pictorial review of the abnormal and unusual. AJR Am J Roentgenol. 2011 Apr;196(4):W451-60. DOI: 10.2214/AJR.10.4864.
- Zingaretti N, Fasano D, Baruffaldi Preis FW, Moreschi C, Ricci S, Massarut S, Ricci S, Massarut S, De Francesco F, Parodi PC. Suspected Breast Implant Rupture: Our Experience, Recommendations on its Management and a Proposal for a Model of Informed Consent. European Journal of Plastic Surgery 43: 569–576 (2020). https://rdcu.be/cLiiU
- Glynn C, Litherland J. Imaging Breast Augmentation and Reconstruction. Br J Radiol. 2008 Jul;81(967):587-95. DOI: 10.1259/bjr/61567884.
- Klang E, Amitai MM, Raskin S, Rozendorn N, Keddel N, Pickovsky J, Sklair-Levy M. Association between Enlarged Axillary Lymph Nodes and Silicone Breast Implant Ruptures seen on Magnetic Resonance Imaging. Isr Med Assoc J. 2016 Dec;18(12):719-724. https://pubmed.ncbi.nlm.nih.gov/28457073/
- Lee Y, Song SE, Yoon ES, Bae JW, Jung SP. Extensive silicone lymphadenopathy after breast implant insertion mimicking malignant lymphadenopathy. Ann Surg Treat Res. 2017 Dec;93(6):331-335. DOI: 10.4174/astr.2017.93.6.331.
- Samreen N, Glazebrook KN, Bhatt A, Venkatesh SK, McMenomy BP, Chandra A, Leng S, Adler KE, McCollough CH. Imaging findings of mammary and systemic silicone deposition secondary to breast implants. Br J Radiol. 2018 Sep;91(1089):20180098. DOI: 10.1259/bjr.20180098.