Spinal Vascular Malformations
Find your care
Our expert team is skilled at treating complex cerebrovascular conditions and providing the finest and most comprehensive patient care. For help finding a neurosurgeon, call 310-825-5111.
Overview
What are spinal vascular malformations?
Spinal vascular malformations include several distinct disorders involving an abnormal connection between arteries and veins around the spinal cord. Four types of spinal vascular malformations are described below; additionally, cavernous malformations and arterial aneurysms are vascular lesions that can also occur in the spine.
Types of spinal vascular malformations
- Spinal Dural Arteriovenous Fistulas (Type I)
-
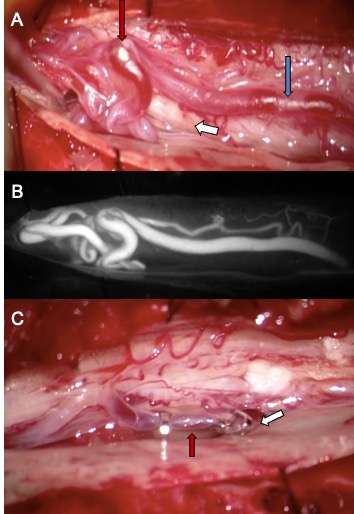
 Figure 1. Type I Spinal Dural Arteriovenous Fistula - Spinal angiogram (left image) of a left sided spinal segmental artery (white arrow) with an abnormal connection (red arrow) to a spinal cord vein that has become abnormally enlarged (blue arrow)
Figure 1. Type I Spinal Dural Arteriovenous Fistula - Spinal angiogram (left image) of a left sided spinal segmental artery (white arrow) with an abnormal connection (red arrow) to a spinal cord vein that has become abnormally enlarged (blue arrow)- These malformations represent 70% of spinal vascular malformations and are the result of an abnormal connection forming between an artery and a vein in the spinal canal dural covering (Figure 1). This connection allows high pressure arterial blood to escape into the low-pressure network of spinal cord veins. Over time, the spinal cord is damaged by the elevated pressure in the veins. Spinal dural arteriovenous fistulas (AVFs) are thought to form spontaneously during adulthood and are not congenital or hereditary. These lesions rarely rupture or bleed, but they do cause significant spinal cord dysfunction that can result in leg weakness, lower body numbness, imbalance, and urinary problems. These malformations are good candidates for surgical treatment and endovascular treatment, which are typically curative.
- Spinal Arteriovenous Malformation (Type II)
- Also called a glomus AVM, type II spinal arteriovenous malformations (AVMs) consist of an abnormal connection between the arteries and veins occurring within the spinal cord itself. The connection takes place in a focused collection of abnormal vessels called the AVM nidus. Spinal AVMs represent about 20% of spinal vascular malformations and can present with bleeding into the spinal fluid, spinal cord, and sudden neurological problems attributed to injury of the spinal cord (for example: lower extremity weakness/paralysis and loss of sensation/numbness). Treatment selection in these cases is a highly nuanced decision-making process.
- Juvenile Arteriovenous Malformations (Type III)
- Juvenile spinal AVMs are rare vascular malformations involving the spinal bones, spinal dural covering and spinal cord itself. These lesions are believed to form in early development before birth and are challenging to treat due to their tendency to be large, high-flow, and involve critical structures.
-
 Figure 2. Type IV Pial Spinal Arteriovenous Fistula – sagittal or side view of a T2 MRI of the spine (left) showing a massively enlarged spinal vein (red arrow) compressing the spinal cord (white arrow).
Figure 2. Type IV Pial Spinal Arteriovenous Fistula – sagittal or side view of a T2 MRI of the spine (left) showing a massively enlarged spinal vein (red arrow) compressing the spinal cord (white arrow).Pial Spinal Arteriovenous Fistulas (Type IV)
- Pial spinal AFVs are a direct connection between an artery and a vein on the surface of the spinal cord. These lesions are very rare and come to attention for various reasons, such as when the vein has become enlarged due to high pressure from the artery and this structure begins to compress the spinal cord (Figure 2).
Symptoms
What are the symptoms of spinal vascular malformations?
Symptoms of spinal vascular malformations vary depending on the type of vascular problem and the level(s) of the spinal cord involved. Detecting spinal AVFs (Type I) is particularly important because if left untreated, patients will slowly lose the use of their legs, but with treatment, the symptoms can be stopped and often reversed. The symptoms of spinal vascular malformations can be broken into two categories: a) progressive spinal cord dysfunction and b) sudden problems due to malformation bleeding.
- Progressive spinal cord dysfunction (progressive myelopathy) – Type I-IV
- Slowly progressive weakness in the legs over months to years
- Development of incontinence of urine
- Inability to walk long distances and imbalance
- Difficulty feeling the legs (numbness)
- Pain (not always)
- Impotence/sexual dysfunction
- Sudden weakness or bleeding into the spinal fluid – Type II
- Spinal AVMs can present with sudden weakness of the legs or arms and legs.
- Sudden severe back pain can be due to a rupture of the abnormal vessels into the spinal fluid. It often happens at exactly the same time as the weakness starts. Bleeding in the spinal fluid can cause:
- Nausea
- Vomiting
- Headache
- Neck stiffness
- Pain in the back, arms, and/or legs
Diagnosis
How are spinal vascular malformations diagnosed?
The diagnosis of a spinal vascular malformation is typically first suspected by physicians based on the patient’s symptoms. Based on the symptoms, the physician may order the following examinations:
- Spinal MRI – This test is typically the first study ordered when a spinal vascular malformation is suspected. Spinal MRIs can demonstrate abnormal enlarged vessels, abnormal spinal cord changes and give important clues about the presence and location of the vascular malformation.
- Spinal angiogram – This exam is the gold standard for confirming the presence of a spinal vascular malformation, characterizing the malformation, and demonstrating its exact location in the spinal canal (Figure 3). This imaging study is used to best understand the anatomy of the malformation so the appropriate treatment option can be determined.
- Spinal MRA or CTA – These tests at experienced centers can demonstrate the presence of vascular malformations and can serve as a screening test. However, they provide less detailed information than a spinal angiogram.
Treatment
What are the treatments for spinal vascular malformations?
The appropriate management and treatment strategy varies depending on the type of spinal vascular malformation and should be carefully considered and tailored to the individual patient by a specialized cerebrovascular neurosurgeon. The majority of cases are treated in one of two ways:
- Surgery – many spinal vascular lesions are best treated with surgery and can be cured with low risk to the patient (Type I lesions). A spinal angiogram is typically needed prior to surgery in order to guide the surgeons to the abnormal vessels. Surgery typically involves a small incision in the back, in order to disconnect the vascular abnormality (Figure 4).
- Endovascular embolization - Some spinal vascular lesions are best treated from within the blood vessels using endovascular embolization. This procedure involves advancing small tubes called catheters within the blood vessels under x-ray guidance and injecting a specially designed type of glue to close the abnormal vessel. Some lesions can be cured with embolization; other lesions may require the abnormal vessels feeding the AVM to be embolized prior to surgery in order to make surgery safer.
- Observation- Some vascular lesions are best observed rather than treated. This is typically the case with large malformations, complex malformations, asymptomatic malformations, or malformations in critical areas of the spinal cord making them high risk for surgery.
Post-operative care and recovery
Surgery or embolization for spinal vascular malformations disease is best performed at specialized cerebrovascular centers like Ronald Reagan UCLA Medical Center where there are expert neurosurgeons, neuroradiologists and highly specialized care.
At UCLA Health neurosciences, we employ highly specialized multidisciplinary health care teams, and in addition to innovative cutting-edge care, we provide support services for patients and their families to help navigate their time in our clinics and hospitals.
Contact us
To schedule an appointment at the UCLA Cerebrovascular Program, please call 310-825-5111 or request a call back for an appointment.

Geoffrey Colby, MD, PhD
Jeremiah Johnson, MD
