About Us

May 2025 - Unit Spotlight: Pathology Facilities & Operations
The Pathology Facilities and Operations team manages facilities, equipment, and safety and compliance for the Department across multiple sites – Westwood, the Bruin University Reference Laboratory (BURL), Santa Monica Medical Center, The UCLA Immunogenetics Center (UIC), Olympic Analytical Lab (OAL) and West Valley Medical Center (WVMC).
The Pathology Facilities and Operations team is comprised of three specialty groups: Pathology Facilities, Pathology Equipment, and Pathology Safety & Compliance. The groups work seamlessly together to maintain operations and execute high-level projects across our multiple locations. They are also a key component for successful department events, ensuring appropriate A/V and technical support and event management. They have supported large-scale events including Research Day and department appreciation events.
The Facilities teams manages Pathology-owned spaces and laboratories, including key/badge access, office/workstation installs, vendor management, furniture procurement, and partnering with University Facilities to address issues/damage requiring work by teams outside of the department.
Pathology Equipment manages department equipment and maintenance, not limited to microscopes, computers, conference rooms, and other required equipment. They also assist with requests for equipment relocation, software requests, and interfaces with ISS and DGIT for seamless workstation installations.
Pathology Safety & Compliance assists with pre-inspection and inspection requests, reporting for Chemical/Biohazardous Spills (post-event), Reporting Accidents (post-incident, research-side only), Laboratory Onboarding/Decommission, Emergency Preparedness, capital lab equipment requests, training, and general safety practices.
The Pathology Facilities and Operations team is a vital part for the Department of Pathology and Laboratory Medicine. They provide essential resources to ensure maximum efficiency within our facilities to foster a safe and productive environment to further our Department’s commitment and UCLA Health’s mission to deliver leading-edge patient care, research, education, and community engagement. Thank you Facilities and Operations team, for all you do to help our Department provide outstanding patient care, research, education and administrative activities!!!
Meet the Team
- Lindy Coe – Manager
- Joe Church – Supervisor
- Emily Irineo – Administrative Assistant III (supports PAS & Facilities)
- Jessica Martinez – Facilities Management Specialist, Pathology Equipment
- Teresa Mejia – Facilities Analyst
- Amari Moore – Facilities Analyst
- Christopher Pang Gonzalez – Safety & Compliance
- Ricardo Zaragoza – Facilities Management Specialist, Pathology Equipment

Current Projects
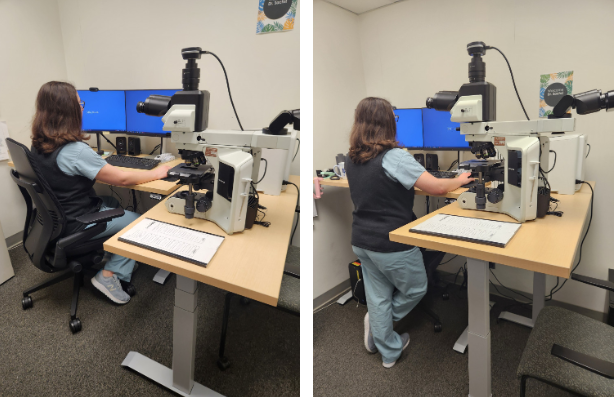
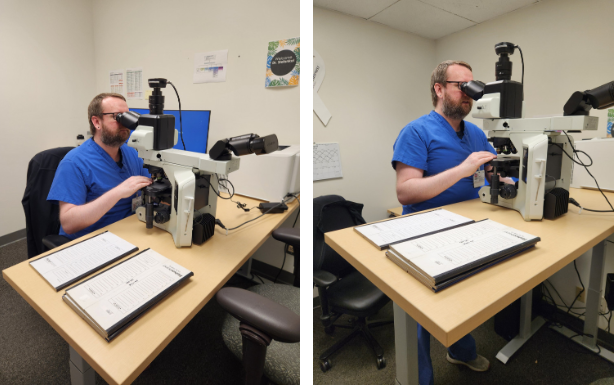
- Height Adjustable Desks for Faculty – Providing options for signout either sitting or standing to enhance workspace ergonomics.
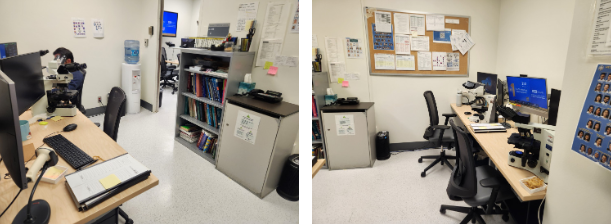
- Hemepath Fellows Room – Enhanced workspace for signout, the Hemepath Fellows, and rotating Trainees.
- Business Office Hoteling Space Breakroom – The addition of the breakroom allows for those in the Business Office to enjoy a lunch space when onsite.
- Fellows Room – The space refresh will include new ergonomic workstations. This project will mirror the successful implementation of the Residents Room this past year


Welcome, Poppy Coe!
You may have noticed you have not seen Lindy Coe, Facilities and Operations and Pathology Administrative Services Manager for Pathology & Laboratory Medicine, on site recently. This is because Lindy has embraced a new and profoundly special project: motherhood. We are thrilled to share that Lindy and her husband, Garth, welcomed their beautiful daughter, Poppy Maureen Coe, into the world on March 20th—two weeks ahead of schedule, eager to meet her loving family.
Lindy has been a cornerstone of our operations, guiding her teams with dedication and expertise. From overseeing vital Facilities projects to deftly managing unforeseen faculty needs, her contributions have been nothing short of exceptional.
Please join me in extending heartfelt congratulations to Lindy and Garth as they embark on this joyous new chapter with baby Poppy.
Sarah M. Dry, MD
Chair, Department of Pathology & Laboratory Medicine
