Dural Arteriovenous Fistula
Find your care
Our interventional neuroradiology team has paved the way for interventional procedures, creating several of the devices and techniques widely used today. Call 310-267-8761 to learn more about our services.
What is dural arterio-venous fistula (DAVF) and how does it occur?
Human brain is covered by three layers of membranes (meninges). The outermost layer of the meninges is a strong menbrane called the dura mater. This dura mater provides essential protection to our brain. There are major venous channels within the dura mater called dural sinuses. The dural sinuses collect blood from veins of the brain. When an abnormal connection is formed between arteries and the dural sinuses, it is called dural arteriovenous fistula (DAVF) / dural arteriovenous malformation / dural fistula. Theoretically, dural arteriovenous fistulas can occur in any part of the dura mater.
Most DAVF's are thought to be an acquired disease. DAVF's can be formed in the following conditions: dural sinus thrombosis (clotting and blockage of the dural sinuses), head injury, and open surgery.
What are the symptoms of DAVF?
The symptoms of DAVFs vary depending on the location of DAVF. Headache is one of the non-specific symptoms that could be associated with all types of DAVFs. Although DAVFs can occur in any part of the location where the dura mater exists, DAVFs are commonly found in cavernous sinus (behind the eye) and transverse / sigmoid sinus (behind the ear, back of your head). Patients with DAVFs behind the eye (cavernous DAVFs) usually complain of decreased vision and redness / congestion / swelling of the eye. Patients with DAVFs behind the ear (transverse / sigmoid DAVFs) frequently hear a pulsating noise (tinnitus) due to the fast blood flow going through the fistulas.
All types of DAVFs can cause stroke-type symptoms and seizures. Brain hemorrhage is the most serious presentation of DAVFs and can cause permanent disability and death. Some DAVFs do not present any symptoms at all. However, severity of the symptoms is not necessarily associated with the risk of brain hemorrhage. For example, DAVFs without any symptoms can cause brain hemorrhage.
How can it be treated?
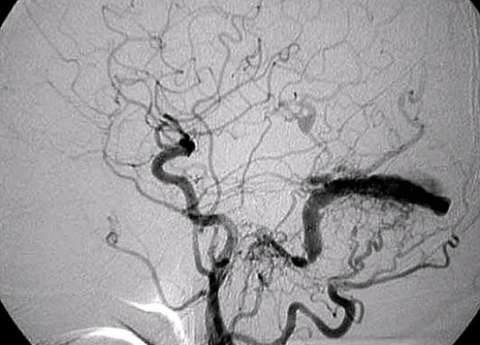
First step of the treatment is to obtain an entire picture of a DAVF and characterize it. Cerebral angiography (dye injection into brain arteries through a plastic tube) is the gold-standard and the most accurate way to do so. Based on the finding of cerebral angiography and the symptoms, the following options are offered:
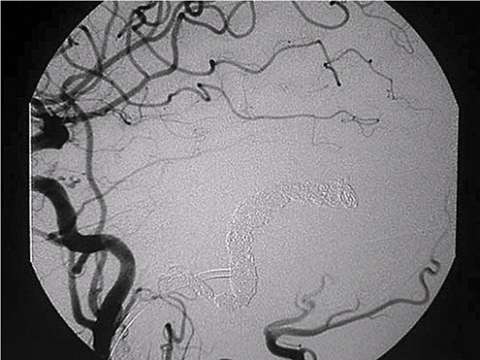
- Endovascular embolization
- Open surgery
- Observation
One of the most worrisome finding is so called "cortical venous reflux". This is the sign that blood flow return to the brain is compromised and associated with high risk of brain hemorrhage. Regardless of the symptoms, DAVF's with cortical venous reflux should be treated as soon as practical by either endovascular embolization or open surgery. Recently, most DAVF's can be treated by endovascular embolization.
When a patient cannot tolerate the symptom such as pulsating noise, endovascular embolization is considered. Simple observation can be an option for some DAVF's with negligible risk of hemorrhage.