Ultrasound: Calcifications
by Brian Tsui, MD, and James Chalfant, MD
Calcifications are less frequently visualized on ultrasound (US) when compared to mammography, with one study demonstrating sonographic visualization in 23% of cases with mammographic calcifications recommended for biopsy1. Mammography remains the best way to characterize calcifications, especially microcalcifications, since US cannot determine their morphology.
However, the identification of calcifications on ultrasound can provide radiologists useful information during a diagnostic evaluation. In a prospective study, suspicious mammographic calcifications that demonstrated sonographically visualized calcifications were more likely to be malignant (69%) and invasive (72%)1.
When calcifications are visualized on US, they typically appear as hyperechoic foci, which may or may not cause shadowing. Doppler US can also be used to detect calcifications, which may demonstrate “twinkling” artifact. Calcifications may be seen within a mass, outside a mass, or within ducts2. When suspicious mammographic calcifications are also visualized on ultrasound, they tend to have a larger number of calcifications and involve a larger area on mammography. In these cases, the calcifications are also most frequently seen associated with a mass on ultrasound, despite there being no mass visualized mammographically1.
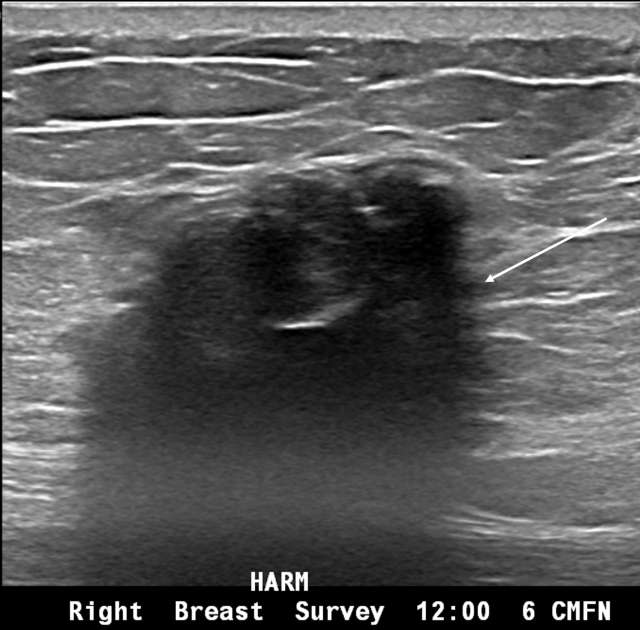
Within a mass, calcifications may appear as hyperechoic foci, typically without posterior acoustic shadowing unless they are larger or coarse.
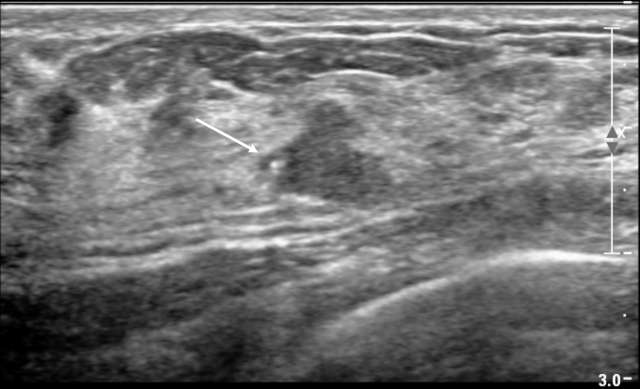
Outside of a mass, calcifications are generally harder to visualize as they may blend in with the hyperechoic speckles in the breast and Cooper ligaments. However, when an abnormal nonmass sonographic finding is identified (defined as a “discrete identifiable area of altered echotexture compared with that of the surrounding breast tissue that does not conform to a mass shape”) and demonstrates associated calcifications, such findings are frequently associated with malignancy3. Studies have shown that calcifications are present in up to 51% of malignant nonmass findings compared to 0-10% in benign nonmass findings3.

Intraductal calcifications are less commonly seen on US but usually represent a suspicious finding that should be biopsied2.
When suspicious calcifications are seen on ultrasound, sonographic guided biopsy can be considered over stereotactic biopsy1. This offers several potential advantages. Stereotactic biopsy can be uncomfortable due to positioning and compression. Furthermore, stereotactic guidance requires the use of ionizing radiation, which ultrasound avoids. Ultrasound can also visualize the needle in real time. Specimen radiography can then be performed to ensure that calcifications are within the biopsy samples.
References:
- Soo MS, Baker JA, Rosen EL. “Sonographic detection and sonographically guided biopsy of breast microcalcifications.” AJR Am J Roentgenol. Apr 2003;180(4):941-8. DOI:10.2214/ajr.180.4.1800941
- D’Orsi C, Sickles E, Mendelson E, Morris E. ACR BI-RADS ® Atlas, Breast Imaging Reporting and Data System. 5 ed. American College of Radiology; 2013.
- Choe J, Chikarmane SA, Giess CS. “Nonmass Findings at Breast US: Definition, Classifications, and Differential Diagnosis.” Radiographics. 2020 Mar-Apr 2020;40(2):326-335. DOI:10.1148/rg.2020190125