In the News
Find your care
Our expert team is skilled at treating complex cerebrovascular conditions and providing the finest and most comprehensive patient care. For help finding a neurosurgeon, call 310-825-5111.
UCLA Cerebrovascular Program News

Actress Keala Settle Celebrates World Moyamoya Day with Thanks to Dr. Anthony Wang and UCLA
In honor of hashtWorld Moyamoya Day, actress Keala Settle spoke about her experience with Moyamoya and shouted out Cerebrovascular Neurosurgeon Dr. Anthony Wang and the UCLA Neurosurgery team.
We are honored to provide top-notch, individualized care to all Moyamoya patients that visit us at UCLA Neurosurgery.
Read Keala's post here.

Neurosurgery Connections - Cerebrovascular Edition
In this edition of the newsletter, we highlight a selection of the innovative research and clinical advancements occurring in our Cerebrovascular Division.
View the Cerebrovascular Edition of Neurosurgery Connections >
UCLA Health Designated as a Center of Excellence for the Treatment of Cavernous Malformations
The Alliance to Cure Cavernous Malformation recently designated UCLA Health as a Cerebral Cavernous Malformation (CCM) Clinical Center. UCLA Health is the only CCM Clinical Center in Southern California.
This designation is awarded to healthcare institutions that offer top-notch interdisciplinary care for both pediatric and adult cavernous malformations.
“The Alliance to Cure Cavernous Malformation is an important resource for patients and families that live with this complex disease, and we have worked side-by-side with them for many years,” said Dr. Anthony Wang. “We are honored to receive this recognition, as we believe that it reflects the elite care, expertise, and dedication that our team at UCLA Health brings to the care of our cavernous malformation patients.”
Cavernous malformations are abnormal groups of small blood vessels that develop in the brain and spinal cord. These clusters increase the risk of stroke, seizures, and brain hemorrhage in otherwise healthy patients. Brain and spinal surgery are the only treatments for cavernous malformations, although medications do exist to strengthen the blood vessels and thus potentially prevent the development of additional cavernous malformations.
The Alliance to Cure Cavernous Malformation is an organization dedicated to providing information and support for patients and families impacted by cavernous malformations. Learn more here.
Here's why Joni Mitchell's performance at the Newport Folk Festival is so incredible
Dr. Anthony Wang is interviewed for NPR
Joni Mitchell's surprise performance at the Newport Folk Festival on Sunday is already becoming the stuff of legend. The unsuspecting crowd roared as the singer-songwriter stepped onto the stage in her first public performance since suffering a debilitating brain aneurysm in 2015. Dr. Anthony Wang, a neurosurgeon at Ronald Reagan UCLA Hospital, is among those who are astounded by Mitchell's recovery. "To be able to recover to the point of being able to perform as a musician is really incredible," Wang told NPR. Brain surgeons often use "return-to-work" as a marker of a successful functional recovery, he explained. "But very rarely is that work quite so nuanced."
UCLA Health's multidisciplinary collaboration expands the breadth of treatment options for complex neurovascular cases
In recent years, neurologists, neurosurgeons, and neuro-radiologists have made huge advances in delivering fast treatment after a stroke, preventing countless deaths and disabilities. Sometimes, however, it pays to not wait for an acute event. For example, patients with intracranial atherosclerotic disease (ICAD) — the narrowing of the large vessels of the arteries leading to the brain, putting them at risk for stroke — benefit from early referral to an expert center, in part because the best course of therapy isn’t always clear.
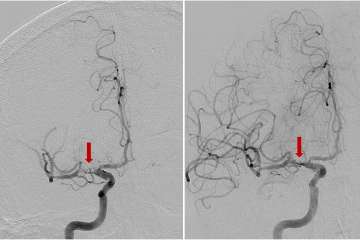
Advances in vascular imaging technology are opening up additional options for stroke prevention and cognitive health. Conditions that reduce the blood flow to the brain, including ICAD and moyamoya disease, can cause recurrent strokes and significant cognitive and neurological impairment. Surgery to re-open or bypass blocked arteries may help, but experience shows that a personalized treatment plan based on imaging and other clinical data is needed to provide patients the best possible outcomes.
The UCLA Stroke Center provides comprehensive diagnostic and therapeutic care for simple and complex vascular disorders through multidisciplinary teams that work closely with patients and their referring physicians. “We offer the expertise not just of individuals, but of our center as a whole,” says neurosurgeon Geoffrey Colby, MD, PhD, director of cerebrovascular neurosurgery at UCLA. “A good part of the success of the procedures we perform comes from the care that’s provided before and after, through the immediate recovery period and beyond.”
Cutting-edge research leads to evidence-based care
In addition to caring for patients, the center’s faculty advance clinical care as leaders in research. “We’re doing a lot of collaborative research across the country and internationally to understand how we can use these advanced tools to better define the disease,” says vascular neurologist David Liebeskind, MD, director of the UCLA Stroke Center. “And not just to define it, but also to treat it.”
Dr. Liebeskind heads a number of ICAD studies to learn more about stroke risk and the impact on cognitive function. Using detailed longitudinal imaging studies, for example, his group is examining how physical activity affects blood pressure and other risk factors to prevent stroke. Through computational fluid dynamics, he and his colleagues are learning how the specific architecture of the narrowing of the vessels might affect stroke risk. Dr. Liebeskind also heads a large NIH-funded study of patients with asymptomatic carotid disease to better understand how blood flow relates to cognition over time, and the potential impact on dementia risk.
“Brain or cerebrovascular health is a relatively novel concept, unlike the established prominence of cardiovascular health,” says Dr. Liebeskind. “Given the impact of ICAD on neurological disability, more detailed clinical and imaging evaluation of these individuals is key to properly tackling this disease.”
The center’s neurosurgeons treat patients with complex vascular lesions, often using revascularization to avert ischemia and then monitoring patients to provide ongoing treatment for the disease. “Vanishingly few health care systems in the world offer a full range of surgical revascularization options for stroke patients,” says neurosurgeon Anthony Wang, MD, who specializes in cerebrovascular, pediatric and complex cranial-base surgeries. “At UCLA, we are able to offer the complete range of surgical revascularization options, and the rare expertise of our team allows us to tailor a plan for each individual patient’s needs.”
Expertise that goes beyond the ‘typical patient’
Moyamoya disease typically affects young people, even children, who are seemingly healthy until the condition is discovered following a stroke. After a stroke, moyamoya patients often “sit at a tipping point,” says Dr. Wang. “They have the potential both for an excellent recovery or for disastrous progression.” To better ensure that a patient tips toward recovery, researchers at UCLA are testing non-invasive interventions to protect vulnerable regions of the brain adjacent to the initial stroke. For instance, stimulation of certain nuclei using high-intensity focused ultrasound appears to have a neuroprotective effect. Transcranial direct-current stimulation is currently in trials for patients with acute strokes caused by large vessel occlusion, and may prove useful for moyamoya patients as well.
Stroke is rare in the overall pediatric population, and the UCLA Stroke Center stands apart for being staffed with experienced neurologists, neurosurgeons and radiologists who subspecialize in treating pediatric stroke, both in the acute and outpatient settings. “It can be challenging to recognize the signs of stroke in children, as the overall incidence is low and the clinical presentation can be nonspecific, particularly in infants,” neurologist Latisha Sharma, MD, says. Once the acute care is completed, access to a team with a multifaceted approach to outpatient treatment of the child in ensuing years plays an essential role in his or her recovery, Dr. Sharma says.
Although stroke is the third-leading cause of death among women in the United States, Dr. Sharma notes that the symptoms can be subtle and are more likely to be missed or minimized by women than men. “We need to do more to educate women to call 911 and not delay seeking treatment especially if there is a sudden neurological change,” she says. Women may be at higher stroke risk in the antenatal and postpartum period from conditions such as preeclampsia. “Preeclampsia is considered a sex-specific risk factor for future stroke but is often underrecognized, and many women are unaware of their risk later in life,” Dr. Sharma adds.
After diagnosis and treatment, ongoing monitoring and management is key
The UCLA Stroke Center’s comprehensive, long-term management approach benefits patients with complex vascular conditions, such as intracranial aneurysms or arteriovenous malformations. “These are patients who need to be followed for life, both to make sure that whatever treatment is offered is durable and to screen them to ensure they’re not developing new aneurysms,” Dr. Colby says.
Once patients are diagnosed — typically following a workup for an unrelated symptom — the decision on how to manage it isn’t always straightforward, Dr. Colby notes. Treatment options can include several types of open surgery, as well as a host of minimally invasive endovascular options.
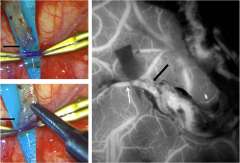
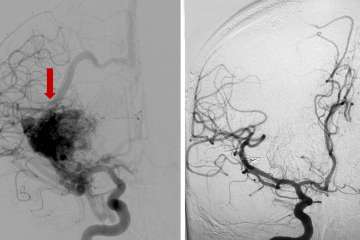
With an arteriovenous malformation, treatment decisions are nuanced and depend on whether the vessel has caused bleeding in the brain or not, says neurosurgeon Jeremiah Johnson, MD. “These complex tangles of blood vessels in the brain can rupture and cause hemorrhagic stroke,” explains Dr. Johnson. “The definitive treatment is surgery to remove the malformation, but sometimes that’s not possible due to location in the brain or other factors. For very deep or critical parts of the brain, for example, we often avoid surgery but may be able to treat with other modalities.”
If the blood vessel malformation hasn’t ruptured, ongoing monitoring can sometimes be the safest option, but each patient and each malformation is different. The preferred option to treat some AVMs may be stereotactic radiation, where radiation beams are tightly focused on the malformation but minimally impacting the surrounding normal tissues. Or it could involve embolization, or blocking off surrounding branches of the blood vessel to safely remove the malformation. UCLA provides individualized expert care for even the most complex cerebrovascular disorders. Both Dr. Johnson and Dr. Colby are dual-trained in endovascular and cerebrovascular open surgery techniques, with expertise to perform these multifaceted procedures.
Collaborative care provides patients with personalized treatment
“We’ve learned a great deal through studies showing that having the full arsenal of surgical techniques is important, given that these patients present differently, and that certain presentations or anatomies respond better to certain treatments,” says Dr. Colby.
Offering the full array of treatment options along with advanced imaging capabilities to guide the decision-making process, the UCLA Stroke Center is well positioned to take on these cases and to provide a customized solution for each patient. “We have multidisciplinary conferences that include specialists in neurosurgery, neurointerventional radiology and cerebrovascular neurology in which we make sure our patients receive optimal management,” Dr. Colby says. “The only way you can do that is if you offer everything and don’t have any biases about one procedure or another.”