Case: Accessory Breast Tissue
Background:
Accessory breast tissue is residual breast tissue that results from failure of regression during embryogenesis.1 It is found in up to 6% of the population with the highest incidence in Japanese populations and the lowest incidence in Caucasians.2 During the 4-6th week of gestation, bands of ectodermal thickening form the mammary ridges or “milk lines,” which extend from the bilateral anterior axillary folds to the medial inguinal folds. A single pair of mammary tissues in the pectoral region persists, while the remaining tissues regress. Thus, accessory breast tissue occurs when there is incomplete regression or displacement of the mammary ridges during embryogenesis.2 While most cases are sporadic, an autosomal dominant inheritance pattern with incomplete penetrance is also proposed2.
Accessory breast tissue is frequently bilateral and most commonly occurs in the axilla, followed by the inframammary area.1 Notably, accessory breast tissue is also reported to occur outside of the mammary ridges in various anatomic locations including the face, posterior neck, mid back, buttocks, vulva, flank, hip, scapula, and upper extremities.2
Terminology and Classification:
Ectopic breast tissue is an umbrella term used interchangeably in the literature to describe accessory, supernumerary, and/or aberrant breast tissue.1 Kajava established a classification system for supernumerary breast tissue based on the presence of nipple, areolar, and glandular tissues3 (Table 1). Class IV is the most common clinical presentation.2 Aberrant breast tissue is defined as unorganized islands of breast tissue, which are located close to the normal breast, but outside of the periphery of the main gland.2
Table 1. Classification of supernumerary breasts established by Kajava in 1915
| Class | Tissue Present |
|---|---|
| I | Nipple, areola, glandular (polymastia) |
| II | Nipple and glandular |
| III | Areola and glandular |
| IV | Glandular |
| V | Nipple and areola (pseudomamma) |
| VI | Nipple (polythelia) |
| VII | Areola (polythelia areolaris) |
| VIII | Patch of hair (polythelia pilosa) |
Clinical Presentation
Most patients with accessory breast tissue are asymptomatic and unaware of its presence. However, because accessory breast tissue is comprised of varying combinations of normal breast tissue, it may respond to hormonal influences. Consequently, clinical symptoms often become evident during pregnancy, lactation, or menarche, and may be associated with the monthly premenstrual phase as well.1
When symptomatic, patients may present with a palpable abnormality associated with pain, swelling, milk secretion, and/or skin erythema.2 Other issues that may arise include limited arm movement and cosmetic concerns.1 During initial clinical evaluation, accessory breast tissue is most commonly confused with or misdiagnosed as lymphadenopathy, lipoma, sebaceous cysts, or malignancy.2
Imaging Appearance:
Accessory breast tissue may be identified as part of a diagnostic exam or incidentally on screening exams.
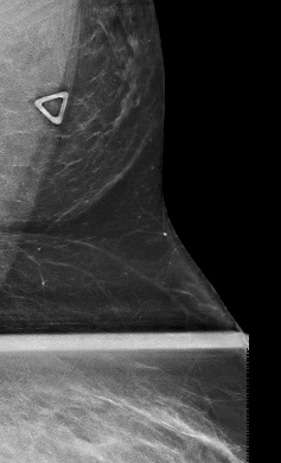
On mammography, accessory breast tissue in the axilla presents as variable quantities of fibroglandular densities scattered amongst fat, which is separate from the main pectoral breast tissue2 (Fig. 1). This appearance should be distinguished from the axillary tail of Spence, which is fibroglandular tissue that is contiguous with the main duct system of the breast tissue and extends into the axilla.1 Of note, if a focal asymmetry in the axilla is new, changed, or identified on a baseline study, a diagnostic exam should be performed to rule out a pathologic process.2
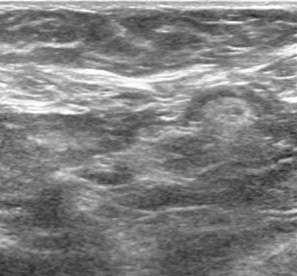
Ultrasound is the primary imaging modality used in the evaluation of lumps outside of the breast or in patients who are less than 30 years of age.2 On ultrasound, accessory breast tissue appears like breast tissue within the main pectoral breast – a mixture of fibroglandular tissue and lobules of fat (Fig. 2).
On MRI, accessory breast tissue may present as an ill-defined mass or non-mass enhancement that is discontinuous with the main pectoral breast tissue, but demonstrates similar signal intensity and contrast enhancement.2
Pathology:
The same disease processes that arise within the pectoral breasts may also occur in accessory breast tissue, including both benign and malignant pathologies. Many benign entities have been reported in accessory breast tissue including lactating adenomas, fibroadenomas, mammary hamartomas, and fat necrosis.1,2
Ectopic breast cancers account for approximately 0.3-0.6% of breast cancers and may occur concurrently with disease in the pectoral breast.2,4 Malignancy within accessory breast tissue most frequently presents as a palpable lump, but can also present as suspicious calcifications within the axilla.2 Like pectoral breast tissue, invasive ductal carcinoma is the most reported pathology in accessory breast tissue.2
Previous studies suggest that there is an increased risk of malignancy in aberrant breast tissue that may be related to a stagnant secretory system.2 However, this conclusion is controversial as other studies have found no supporting evidence.2
Treatment:
Treatment is unnecessary in most cases of accessory breast tissue. However, if there are bothersome clinical symptoms or cosmetic concerns, surgical excision or liposuction may be pursued.4 Malignancy identified within accessory breast tissue has a worse prognosis in comparison to pectoral breast cancer.4 This is hypothesized to be unrelated to the biologic profile of the cancer, and more likely related to delayed diagnosis in the setting of an atypical presentation and less clinical suspicion.4
Conclusion:
It is essential for radiologists to be aware of the imaging appearance and potential clinical presentations of accessory breast tissue to avoid misdiagnosis of this normal variant. Likewise, being mindful of the various benign and malignant processes that may occur in accessory breast tissue is also critical in guiding further diagnostics, consultation, and/or treatment.
References:
- Lim, HS, Kim, SJ, Baek, JM, Kim, JW, Shin, SS, Seon, HJ, Heo, SH. (2017). "Sonographic Findings of Accessory Breast Tissue in Axilla and Related Diseases." J Ultrasound Med. 2017 Jul;36(7):1469-1478. DOI: 10.7863/ultra.16.06056.
- Thasanabanchong, P., Vongsaisuwon, M. (2020). "Unexpected Presentation of Accessory Breast Cancer Presenting as a Subcutaneous Mass at Costal Ridge: A Case Report." J Med Case Rep. 2020 Mar 31;14(1):45. DOI: 10.1186/s13256-020-02366-0.
- Patel PP, Ibrahim AM, Zhang J, Nguyen JT, Lin SJ, Lee BT. "Accessory Breast Tissue." Eplasty. 2012;12:ic5. PMCID: PMC3336208
- DeFilippis, EM, Arleo, EK. "The ABCs of Accessory Breast Tissue: Basic Information Every Radiologist Should Know." AJR Am J Roentgenol. 2014 May;202(5):1157-62. DOI: 10.2214/AJR.13.10930.