Post-Surgical Fluid Collections: Causes, Symptoms, and Management
by Hiro Sparks, M.D. and Tejas C. Manchandia M.D.
Accumulation of fluid within the breast following surgery is relatively common. Potential complications of these fluid collections and their management requires accurate diagnosis of the underlying pathophysiology. Post-operative fluid collections can be broadly categorized as infectious, hemorrhagic, or inflammatory. This article explores the causes, symptoms, imaging appearance, and treatment strategies for post-operative breast fluid collections.
Infection/Abscess
- Background
- Higher incidence with diabetes, obesity, older age (>65 years), nicotine users, prior radiation, or chemotherapy.1-3
- Infection following breast cancer surgery occur in approximately 0.5-2%, of patients although rates as high as 35% have been reported when immediate implant reconstruction is performed.3-5
- Large seromas or hematomas increase risk of postoperative breast infections.4,6
- Usually occur within 1 to 2 weeks following surgery.7 Subacute (months) and late (months to years) infections may occur although uncommon.4
- Clinical Presentation
- Fluctuant, tender mass at the surgical site. Overlying erythema, warmth, and/or edema is common. Systemic symptoms such as fever and tachycardia may also be present.
- Imaging Appearance
US: Complicated hypoechoic or isoechoic fluid collection. Mobile debris within the fluid collection and hypervascularity of the adjacent breast tissue are characteristic, Figure 1.7
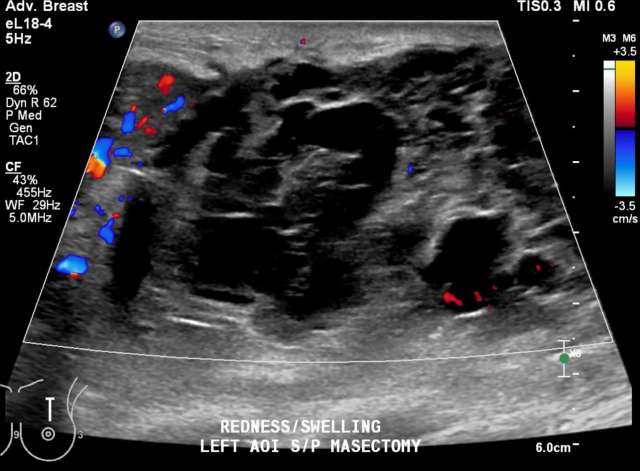 Figure 1 - Ultrasound demonstrates septated, heterogenous fluid collection with surrounding hypervascularity. The patient was 3 weeks status post mastectomy and presented with breast redness and tenderness. The collection was drained, with cultures growing staph aureus.
Figure 1 - Ultrasound demonstrates septated, heterogenous fluid collection with surrounding hypervascularity. The patient was 3 weeks status post mastectomy and presented with breast redness and tenderness. The collection was drained, with cultures growing staph aureus.- CT: Low-attenuation fluid collection with thick/irregular enhancing wall.
- Treatment
- Oral antibiotics are usually first line therapy. Staphylococcus aureus is the most common organism and can be treated with dicloxacillin or first-generation cephalosporin. If MRSA is suspected, broader spectrum antibiotics are required.8
- Percutaneous aspiration should be attempted if the collection is amenable to drainage. Following aspiration, symptoms resolve without surgery in 54-100% of cases.9, 10
- Failure of percutaneous drainage has been associated with large abscess cavity >5cm, presence of multiple loculations, delayed presentation (i.e. symptoms >6 days).8
- In cases where percutaneous aspiration fails, surgical incision and drainage should be attempted.8
- In cases involving prosthetic implants, superficial infections may be treated with antibiotics. Deep infections involving the implant usually require surgical management.3
Hematoma
- Background
- Rare postsurgical complication, with incidence of 2–10%. 11
- Likely arise from uncauterized vessels.
- NSAIDS, aspirin, fish oil may increase risk of developing a postoperative hematoma. 12
- Clinical Presentation
- May be asymptomatic. When symptomatic, may present with pain and overlying skin ecchymosis.11
- Imaging Appearance
US: Heterogenous fluid collection with fluid-fluid level, Figure 2.
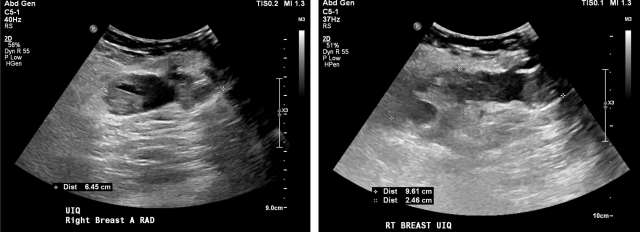 Figure 2 - Ultrasound demonstrating post-surgical hematoma of the right breast. Heterogenous fluid collection with fluid-fluid level (yellow arrow). There was ecchymosis overlying the area of interest in the upper inner quadrant.
Figure 2 - Ultrasound demonstrating post-surgical hematoma of the right breast. Heterogenous fluid collection with fluid-fluid level (yellow arrow). There was ecchymosis overlying the area of interest in the upper inner quadrant.- CT: Variable appearance depending on age. Usually appears as a heterogenous breast mass with higher attenuation fluid early with progression to simple fluid attenuation as it evolves. There should be no solid-tissue component or internal enhancement.7
MRI: Variable T1/T2 appearance depending on chronicity. High intensity unenhanced T1 appearance with fluid-fluid level (hematocrit level) is characteristic. May demonstrate low-signal intensity hemosiderin rim on T2, Figure 3.7
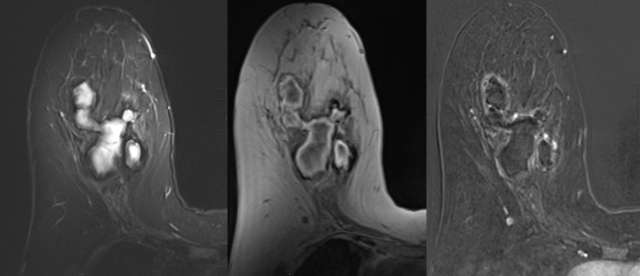 Figure 3 - STIR, T1, and contrast enhanced digital subtraction MRI of the right breast 5 weeks following biopsy. STIR hyperintensity, T1 intrinsic hyperintensity, mild rim enhancement are characteristic of hematoma.
Figure 3 - STIR, T1, and contrast enhanced digital subtraction MRI of the right breast 5 weeks following biopsy. STIR hyperintensity, T1 intrinsic hyperintensity, mild rim enhancement are characteristic of hematoma.
- Treatment
- Small hematomas will gradually resolve with conservative symptom management and observation.
- Large hematomas may require surgical evaluation.
Seroma
- Background
- A seroma is the result of abnormal accumulation of serous fluid in a dead space containing plasma and lymphatic fluid.13
- The underlying pathophysiology for seroma formation is unclear, and likely multifactorial. Fluid accumulation may directly result in part from transected blood and lymphatic vessels during extensive soft tissue dissection. Additionally, significant resection of soft tissue results in a larger potential dead space, causing failure of flap apposition and adherence. Ongoing shearing forces between tissue surfaces may contribute to an inflammatory process with exudative fluid contributing to seroma formation.
- Multiple studies have implicated seroma fluid to contain both lymphatic and inflammatory exudative type fluid.14-16
- More common with mastectomy (20-50% incidence) relative to lumpectomy (9-20% incidence).17
- Prevention of post-surgical seroma via modification flap fixation techniques, application of chemical agents, and insertion of intra-operative drains has yielded mixed results.18
- Clinical Presentation
- Increase risk for wound dehiscence and infection. 19
- Following breast reconstruction surgery, implant loss rates due to seroma have been reported between 2-8%.20,21
- Chronic, untreated seromas may form a dense capsule of fibrous tissue and degenerated hyaline collagen, also referred to as pseudocyst.22
- Although often asymptomatic, seromas may cause pain, anxiety, and functional limitations.
- Increase risk for wound dehiscence and infection. 19
- Imaging Appearance
US: Anechoic simple fluid collections. Complicated fluid collections with heterogenous echogenicity are also possible, Figure 4.17
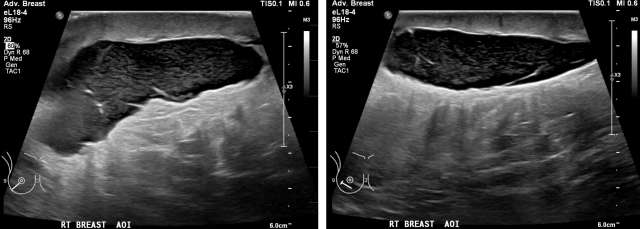 Figure 4 - Homogenous hypoechoic fluid collection with internal debris, compatible with seroma. Smooth, well circumscribed walls without surrounding hypervascularity make abscess less likely.
Figure 4 - Homogenous hypoechoic fluid collection with internal debris, compatible with seroma. Smooth, well circumscribed walls without surrounding hypervascularity make abscess less likely.- CT: Low-attenuation fluid collection without internal enhancement.7
Mammogram: Water-density masses located at the surgical site, Figure 5.23
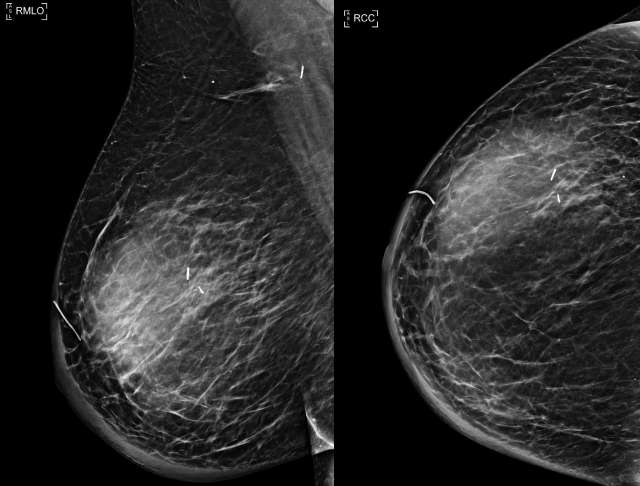 Figure 5 -Right MLO and CC views demonstrate a mass in the upper outer breast 9 months following lumpectomy and sentinel lymph node biopsy. Note prominent skin thickening, which corresponds to patient’s lymphedema.
Figure 5 -Right MLO and CC views demonstrate a mass in the upper outer breast 9 months following lumpectomy and sentinel lymph node biopsy. Note prominent skin thickening, which corresponds to patient’s lymphedema.MRI: Usually a well-defined, homogenous cystic lesion which is hyperintense on T2 and hypointense on T1. Up to 25% have intrinsic T1 hyperintensity due to proteinaceous debris and/or heterogenous contents on T2 images, Figure 6.24
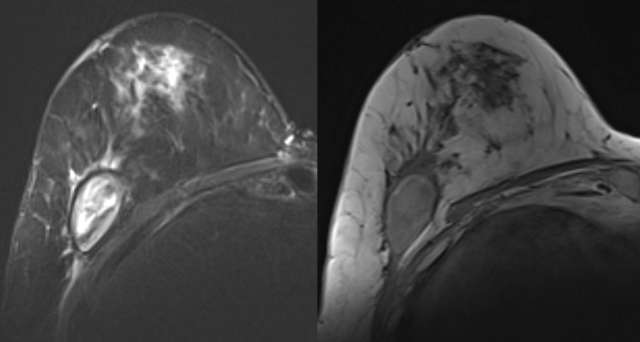 Figure 6 - Seroma is noted on STIR and T1 MRI of the right breast. The fluid collection is STIR heterogenous and T1 hypointense suggesting predominantly simple fluid. Mild edema and post-surgical change is noted in the anterior breast.
Figure 6 - Seroma is noted on STIR and T1 MRI of the right breast. The fluid collection is STIR heterogenous and T1 hypointense suggesting predominantly simple fluid. Mild edema and post-surgical change is noted in the anterior breast.
- Treatment
- Consider conservative management and observation for seromas that are minimal in volume, asymptomatic, and where tension on the surgical wound closure is absent. In most cases, these will reabsorb without the need for further intervention.
- The use of compressive dressings/garments is controvertial,.25,26
- Aspiration is indicated for symptomatic seromas. Ultrasound guidance is preferred especially in peri-prosthetic fluid collections to reduce risk of implant rupture.
- Large volume seromas >75 mL are more often symptomatic.27
- In the special case of prosthetic breast reconstructive surgery, the risk of introducing infection with subsequent implant loss must be weighed against the patient's symptoms, risk of wound dehiscence/necrosis, and the degree of aesthetic effect on the reconstruction.28,29 Decision to drain peri-prosthetic seromas should be made with the referring surgeon.
- Multiple aspirations may be required in cases where re-accumulation of fluid occurs.
- Surgical drainage may be required in cases where encapsulated pseudocyst forms or where there is superimposed infection.27
References:
- Xue DQ, Qian C, Yang L, Wang XF. "Risk Factors for Surgical Site Infections after Breast Surgery: A Systematic Review and Meta-analysis." Eur J Surg Oncol. 2012 May;38(5):375-81. DOI: 10.1016/j.ejso.2012.02.179. Epub 2012 Mar 14. PMID: 22421530.
- Sørensen LT, Hørby J, Friis E, Pilsgaard B, Jørgensen T. "Smoking as a Risk Factor for Wound Healing and Infection in Breast Cancer Surgery." Eur J Surg Oncol. 2002 Dec;28(8):815-20. DOI: 10.1053/ejso.2002.1308. Erratum in: Eur J Surg Oncol. 2003 Jun;29(5):482. PMID: 12477471.
- Stewart CN, Liu BB, Zheng EE, Tuttle SC. "Periprosthetic Fluid Analysis in the Diagnosis of Breast Implant Infections Using Cell Count and Differential." Aesthet Surg J Open Forum. 2020 Jun 12;2(3):ojaa028. DOI: 10.1093/asjof/ojaa028. PMID: 33791651; PMCID: PMC7671253.
- Alderman AK, Wilkins EG, Kim HM, Lowery JC. "Complications in Postmastectomy Breast Reconstruction: Two-year Results of the Michigan Breast Reconstruction Outcome Study." Plast Reconstr Surg. 2002 Jun;109(7):2265-74. DOI: 10.1097/00006534-200206000-00015. PMID: 12045548.
- Jonczyk MM, Jean J, Graham R, Chatterjee A. "Trending Towards Safer Breast Cancer Surgeries? Examining Acute Complication Rates from A 13-Year NSQIP Analysis." Cancers (Basel). 2019 Feb 21;11(2):253. DOI: 10.3390/cancers11020253. PMID: 30795637; PMCID: PMC6407023.
- Mukesh MB, Barnett G, Cumming J, Wilkinson JS, Moody AM, Wilson C, Wishart GC, Coles CE. "Association of Breast Tumour Bed Seroma with Post-operative Complications and Late Normal Tissue Toxicity: Results from the Cambridge Breast IMRT Trial." Eur J Surg Oncol. 2012 Oct;38(10):918-24. DOI: 10.1016/j.ejso.2012.05.008. Epub 2012 Jun 14. PMID: 22704052.
- Neal CH, Yilmaz ZN, Noroozian M, Klein KA, Sundaram B, Kazerooni EA, Stojanovska J. "Imaging of Breast Cancer-related Changes After Surgical Therapy." AJR Am J Roentgenol. 2014 Feb;202(2):262-72. DOI: 10.2214/AJR.13.11517. PMID: 24450664.
- Rao R, Ludwig K, Bailey L, Berry TS, Buras R, Degnim A, Fayanju OM, Froman J, Golesorkhi N, Greenburg C, Ma AT, Mautner SK, Krontiras H, Sowden M, Wexelman B, Landercasper J. "Select Choices in Benign Breast Disease: An Initiative of the American Society of Breast Surgeons for the American Board of Internal Medicine Choosing Wisely® Campaign." Ann Surg Oncol. 2018 Oct;25(10):2795-2800. DOI: 10.1245/s10434-018-6584-5. Epub 2018 Jul 2. PMID: 29968026; PMCID: PMC6512861.
- Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L. "Breast Abscesses: Evidence-based Algorithms for Diagnosis, Management, and Follow-up." Radiographics. 2011 Oct;31(6):1683-99. DOI: 10.1148/rg.316115521. PMID: 21997989.
- Lam E, Chan T, Wiseman SM. "Breast Abscess: Evidence Based Management Recommendations." Expert Rev Anti Infect Ther. 2014 Jul;12(7):753-62. DOI: 10.1586/14787210.2014.913982. Epub 2014 May 3. PMID: 24791941.
- Vitug AF, Newman LA. "Complications in Breast Surgery." Surg Clin North Am. 2007 Apr;87(2):431-51, x. DOI: 10.1016/j.suc.2007.01.005. PMID: 17498536.
- Stanger MJ, Thompson LA, Young AJ, Lieberman HR. "Anticoagulant Activity of Select Dietary Supplements." Nutr Rev. 2012 Feb;70(2):107-17. DOI: 10.1111/j.1753-4887.2011.00444.x. PMID: 22300597.
- Agrawal A, Ayantunde AA, Cheung KL. "Concepts of Seroma Formation and prevention in Breast Cancer Surgery." ANZ J Surg. 2006 Dec;76(12):1088-95. DOI: 10.1111/j.1445-2197.2006.03949.x. PMID: 17199696.
- Andrades P, Prado A, Danilla S, Guerra C, Benitez S, Sepulveda S, Sciarraffia C, De Carolis V. "Progressive Tension Sutures in the Prevention of Postabdominoplasty Seroma: A Prospective, Randomized, Double-blind Clinical Trial." Plast Reconstr Surg. 2007 Sep 15;120(4):935-946. DOI: 10.1097/01.prs.0000253445.76991.de. PMID: 17805122.
- Klink CD, Binnebösel M, Lucas AH, Schachtrupp A, Klinge U, Schumpelick V, Junge K. "Do Drainage Liquid Characteristics Serve as Predictors for Seroma Formation After Incisional Hernia Repair?" Hernia. 2010 Apr;14(2):175-9. DOI: 10.1007/s10029-009-0603-1. Epub 2009 Dec 10. PMID: 19998048.
- Tadych K, Donegan WL. "Postmastectomy Seromas and Wound Drainage." Surg Gynecol Obstet. 1987 Dec;165(6):483-7. PMID: 3686312.
- Neal CH, Pujara AC, Srinivasan A, Chenevert TL, Malyarenko D, Khalatbari S, Helvie MA, Noroozian M, Jeruss JS, Pearlman MD, Davenport MS. "Prospective Imaging Trial Assessing Gadoteridol Retention in the Deep Brain Nuclei of Women Undergoing Breast MRI". Acad Radiol. 2020 Dec;27(12):1734-1741. DOI: 10.1016/j.acra.2020.01.007. Epub 2020 Feb 24. PMID: 32107123.
- Srivastava V, Basu S, Shukla VK. "Seroma Formation After Breast Cancer Surgery: What We Have Learned in the Last Two Decades." J Breast Cancer. 2012 Dec;15(4):373-80. DOI: 10.4048/jbc.2012.15.4.373. Epub 2012 Dec 31. PMID: 23346164; PMCID: PMC3542843.
- Unalp HR, Onal MA. "Analysis of Risk Factors Affecting the Development of Seromas Following Breast Cancer Surgeries: Seromas Following Breast Cancer Surgeries." Breast J. 2007 Nov-Dec;13(6):588-92. DOI: 10.1111/j.1524-4741.2007.00509.x. PMID: 17983401.
- Radu MA, Blidaru A. "Persistent Seroma, a Threat to Implant-Based Breast Reconstruction?" Chirurgia (Bucur). 2021 Mar-Apr;116(2):201-208. DOI: 10.21614/chirurgia.116.2.201. PMID: 33950816.
- Berna G, Cawthorn SJ, Papaccio G, Balestrieri N. "Evaluation of a Novel Breast Reconstruction Technique Using the Braxon® Acellular Dermal Matrix: A New Muscle-sparing Breast Reconstruction." ANZ J Surg. 2017 Jun;87(6):493-498. DOI: 10.1111/ans.12849. Epub 2014 Sep 29. PMID: 25266930.
- Fosheim K, Bojesen S, Troestrup H, Laenkholm AV. "Capsulectomy Can Successfully Treat Chronic Encapsulated Breast Seroma: A Case Report." Cureus. 2022 Jan 27;14(1):e21677. DOI: 10.7759/cureus.21677. PMID: 35237476; PMCID: PMC8882229.
- Soo MS, Williford ME. "Seromas in the Breast: Imaging Findings." Crit Rev Diagn Imaging. 1995;36(5):385-440. PMID: 8540992.
- Davies AM, Hall AD, Strouhal PD, Evans N, Grimer RJ. "The MR Imaging Appearances and Natural History of Seromas Following Excision of Soft Tissue Tumours." Eur Radiol. 2004 Jul;14(7):1196-202. DOI: 10.1007/s00330-004-2255-y. Epub 2004 Mar 9. PMID: 15007612.
- Fabro EAN, Teodózio CGC, Costa RM, Macedo FO, Cardoso ACDDLM, Jacob RBE, Thuler LCS, Bergmann A. "Clinical Experience with Compression Taping to Treat Seroma After Breast Cancer Surgery: A Medical Device Clinical Study." Adv Skin Wound Care. 2022 Jul 1;35(7):1-6. DOI: 10.1097/01.ASW.0000831068.34587.3d. PMID: 35723961.
- Sampathraju S, Rodrigues G. "Seroma Formation After Mastectomy: Pathogenesis and Prevention." Indian J Surg Oncol. 2010 Dec;1(4):328-33. DOI: 10.1007/s13193-011-0067-5. Epub 2011 Apr 2. PMID: 22693384; PMCID: PMC3244263.
- Turner EJ, Benson JR, Winters ZE. "Techniques in the Prevention and Management of Seromas After Breast Surgery." Future Oncol. 2014 May;10(6):1049-63. DOI: 10.2217/fon.13.257. PMID: 24941989.
- Moyer KE, Potochny JD. "Technique for Seroma Drainage in Implant-based Breast Reconstruction." J Plast Reconstr Aesthet Surg. 2012 Dec;65(12):1614-7. DOI: 10.1016/j.bjps.2012.06.016. Epub 2012 Jul 6. PMID: 22770571.
- Brzezienski MA, Jarrell JA 4th, Mooty RC. "Classification and Management of Seromas in Immediate Breast Reconstruction Using the Tissue Expander and Acellular Dermal Matrix Technique." Ann Plast Surg. 2013 May;70(5):488-92. DOI: 10.1097/SAP.0b013e31827eac93. PMID: 23542848.