Case: Metastasis to the Breast From a Non-breast Primary Cancer
By: Margit Szabari, MD, PhD, Hannah Milch, MD, James Chalfant, MD
Metastasis to the breast from a non-breast primary cancer is a very rare condition with a prevalence 1.2% of all malignant tumors in the breast (1). If this rare event occurs, approximately 25% of patients have bilateral breast involvement and about 5% have axillary lymph node involvement (2, 3). Melanoma and pulmonary malignancies are the most frequent primary tumors that metastasize to the breast (4); less frequently seen primary tumors are ovarian, gastrointestinal, thyroid, renal cancer, and sarcomas (5). Interestingly, during adolescence (6), more frequent metastasis to the breast from non-breast cancers has been reported, likely due to hormonal changes. Metastatic rhabdomyosarcoma to the breast has been reported in children (7). In males, prostate is the most frequent primary malignancy to metastasize to the breast (8).
In cases of metastasis to the breast from a non-breast primary tumor, the first line treatment includes chemotherapy, radiation therapy and/or palliative care, while in cases of primary breast cancer, surgical therapy is the standard of care. Therefore, knowing the diagnosis of primary breast cancer versus metastatic disease can save the patient from undergoing unnecessary procedures, can improve morbidity, and change the prognosis. However, making the correct diagnosis can be quite challenging, especially, when the breast mass is the first presentation of a non-breast primary tumor (1).
The typical clinical presentation of metastasis to the breast includes a palpable mass which grows rapidly and generally indicates a wide-spread dissemination of the disease (1). Nipple changes, pain or tenderness are not typical. Close attention should be paid to the past medical history, especially when the patient has had cancer.
Specific Findings Based On Different Imaging Modalities:
-
Mammogram:
Mammography is the first line imaging modality to assess breast masses in women over the age of 30. The majority of metastases present as a round circumscribed mass, either isodense or high density. Calcifications and other mammographic findings are rare. A subset of cases will have no mammographic abnormalities (2). -
Ultrasound:
Generally metastatic disease to the breast can happen via two routes: hematogenous or lymphocytic spread (11):- Typical imaging features of hematogenous metastatic disease include:
Metastatic breast masses from a non-breast primary frequently occur in the upper outer quadrant subcutaneous tissue, likely due to generous blood supply to this area (11). These masses are single or multiple lesions, hypoechoic round or oval well-circumscribed masses, without desmoplastic reaction. Interestingly, features of malignant findings such as calcifications, architectural distortion or spiculations are not typical, however increased vascularity on Doppler images can be seen more frequently. - Typical imaging features of lymphatic metastatic disease:
Lymphatic breast metastases frequently cause skin thickening due to lymphedema, lymph node involvement, and lymphatic dilatation, resulting in diffusely hyperechoic subcutaneous fat and glandular tissue with a thickened trabecular pattern likely due to mechanical obstruction of lymphatics by the mass.
- Typical imaging features of hematogenous metastatic disease include:
-
MRI:
Breast metastases most commonly present as a round or oval mass with smooth margins on MRI (2, 10). Data on enhancement patterns and kinetic analysis is mixed. Surov et al in 2011 (2) demonstrated that more than 80% of breast metastases had type II and type III kinetics curves. On the other hand, Wienbeck et al in 2016 (10) reported slow initial enhancement in a majority of lesions (58%), which would be typical for benign lesions.
Case and Image Presentations From Our Database:
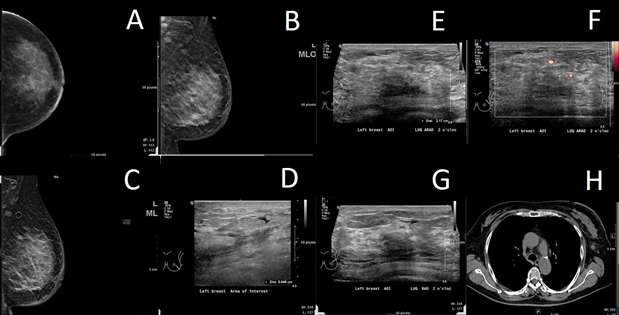
Case 1:
Breast metastasis from biopsy-proven ovarian carcinoma:
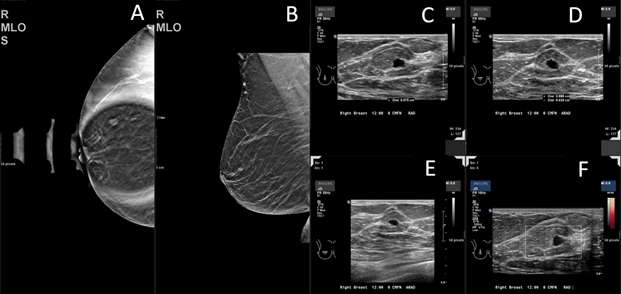
Case 2:
Breast metastasis from melanoma to an intramammary lymph node 5 years after the initial tumor was identified:
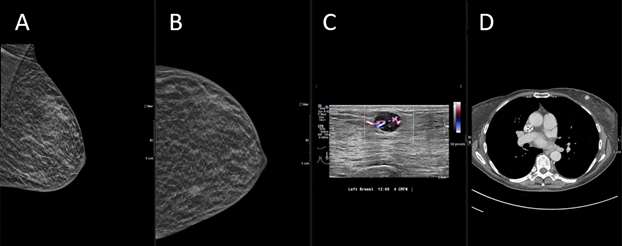
Case 3:
Breast metastasis from possible appendiceal carcinoid tumor:
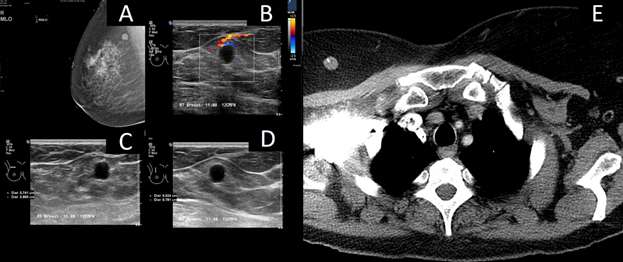
Case 4:
Biopsy proven breast metastasis from retroperitoneal leiomyosarcoma with additional metastasis to the liver and lungs:
References:
- Hajdu SI, Urban JA. "Cancers Metastatic to the Breast." Cancer. 1972 Jun;29(6):1691-6. DOI: 10.1002/1097-0142(197206)29:6<1691::aid-cncr2820290637>3.0.co;2-4. PMID: 4337956.
- Surov A, Fiedler E, Holzhausen HJ, Ruschke K, Schmoll HJ, Spielmann RP. "Metastases to the Breast From Non-mammary Malignancies: Primary Tumors, Prevalence, Clinical Signs, and Radiological Features." Acad Radiol. 2011 May;18(5):565-74. DOI: 10.1016/j.acra.2010.12.009. Epub 2011 Mar 9. PMID: 21393030
- Qureshi SS, Shrikhande SV, Tanuja S, Shukla PJ. "Breast Metastases of Gastric Signet Ring Cell Carcinoma: A Differential Diagnosis with Primary Breast Signet Ring Cell Carcinoma." J Postgrad Med. 2005 Apr-Jun;51(2):125-7. PMID: 16006706.
- Sippo DA, Kulkarni K, Carlo PD, Lee B, Eisner D, Cimino-Mathews A, Harvey SC. "Metastatic Disease to the Breast from Extramammary Malignancies: A Multimodality Pictorial Review." Curr Probl Diagn Radiol. 2016 May-Jun;45(3):225-32. DOI: 10.1067/j.cpradiol.2015.07.001. Epub 2015 Jul 4. PMID: 26293973.
- Sun P, Chen J, Lu J, Luo R, Li M, He J. "Characteristics of Breast Metastases from Non-breast Solid Tumors in 22 Patients from a Southern Chinese Population." Oncol Lett. 2018 Mar;15(3):3685-3693. DOI: 10.3892/ol.2018.7741. Epub 2018 Jan 8. PMID: 29467888; PMCID: PMC5795931.
- Kebudi R, Koc BS, Gorgun O, Celik A, Kebudi A, Darendeliler E. "Breast Metastases in Children and Adolescents with Rhabdomyosarcoma: A Large Single-Institution Experience and Literature Review." J Pediatr Hematol Oncol. 2017 Jan;39(1):67-71. DOI: 10.1097/MPH.0000000000000680. PMID: 27820124.
- Kwan WH, Choi PH, Li CK, Shing MK, Chik KW, Yuen P, Chow LT. "Breast Metastasis in Adolescents with Alveolar Rhabdomyosarcoma of the Extremities: Report of Two Cases." Pediatr Hematol Oncol. 1996 May-Jun;13(3):277-85. DOI: 10.3109/08880019609030828. PMID: 8735345.
- Moldwin RM, Orihuela E. "Breast Masses Associated with Adenocarcinoma of the Prostate." Cancer. 1989 Jun 1;63(11):2229-33. DOI: 10.1002/1097-0142(19890601)63:11<2229::aid-cncr2820631129>3.0.co;2-q. PMID: 2720573.
- Lyou CY, Yang SK, Choe DH, Lee BH, Kim KH. "Mammographic and Sonographic Findings of Primary Breast Lymphoma." Clin Imaging. 2007 Jul-Aug;31(4):234-8. DOI: 10.1016/j.clinimag.2007.02.028. PMID: 17599616.
- Wienbeck S, Herzog A, Kinner S, Surov A. "Magnetic Resonance Imaging Findings of Intramammary Metastases." Clin Imaging. 2016 May-Jun;40(3):361-4. DOI: 10.1016/j.clinimag.2015.12.014. Epub 2016 Jan 21. PMID: 27133668.
- Mun SH, Ko EY, Han BK, Shin JH, Kim SJ, Cho EY. "Breast Metastases From Extramammary Malignancies: Typical and Atypical Ultrasound Features." Korean J Radiol. 2014 Jan-Feb;15(1):20-8. DOI: 10.3348/kjr.2014.15.1.20. Epub 2014 Jan 8. PMID: 24497788; PMCID: PMC3909857.