Case: Lymphoma of the Breast
by Michelle Bondero, MD and Reza Fardanesh, MD.
Introduction, Demographics, Clinical Presentation
Lymphoma is a type of blood cancer that can be seen throughout different parts of the body. Lymphoma in the breast is relatively rare, with a prevalence as low as 0.04-0.7%. This is thought to be due to a low level of lymphoid tissue in the breast. Breast lymphoma can be divided into two categories: primary (PBL) and secondary breast lymphoma (SBL).
PBL is defined as lymphoma that begins in the breast tissue, without previous diagnosis of lymphoma outside of the breast or evidence of widespread disease. There are several types of lymphoma, but the type typically seen in PBL is almost always Non-Hodgkin Lymphoma. Other types seen in PBL that are not as common are follicular lymphoma, mucosa-associated lymphoid tissue lymphoma, and Burkitt lymphoma.
SBL is the most common type of metastasis to the breast, specifically from Diffuse Large B-Cell Lymphoma. SBL can have multiple lesions and bilateral breast involvement.
Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) is a third type of lymphoma to be aware of in the breast. It is rare, affecting between 1 in 1000 and 1 in 10,000. As its name suggests, it is associated with breast implants and can present as a peri-implant fluid collection and/or a breast mass. Studies have shown that the majority of BIA-ALCL cases occur in people with textured implant envelopes, regardless of whether silicone or saline implants are used. Peri-implant fluid collections that appear more than 1 year after placement should be investigated. Typical onset of symptoms is 8-10 years after implant placement. After infectious causes are ruled out, the peri-implant fluid should be aspirated under ultrasound and sent for cytology.
Clinical Presentation
PBL usually presents around ages 60-65 years old, while SBL typically presents between ages 60-70. There are overlapping clinical presentations of PBL and SBL. Some patients report a painless mass that gets bigger over time. In cases of high-grade lymphoma, it is also possible to see inflammatory signs like skin retraction and redness. Sometimes patients may feel pain in their breasts or enlarged lymph nodes. Nipple retraction is a rare finding in breast lymphoma.
Imaging Features
Diagnosing lymphoma solely based on imaging features can be difficult as lymphoma in the breast can present similar to invasive ductal carcinoma and invasive lobular carcinoma. However, differentiating between PBL and SBL is more straightforward. Compared to a SBL, a PBL usually presents as a solitary abnormality on mammography and ultrasound, with or without axillary lymphadenopathy. PBL masses are typically larger than SBLs, the mean diameter being between 2.3-4.6 cm compared to 1.1-2.8 cm in SBL. In a patient with known lymphoma outside of the breast, with multiple masses in the breast or breast skin thickening are suggestive of SBL.
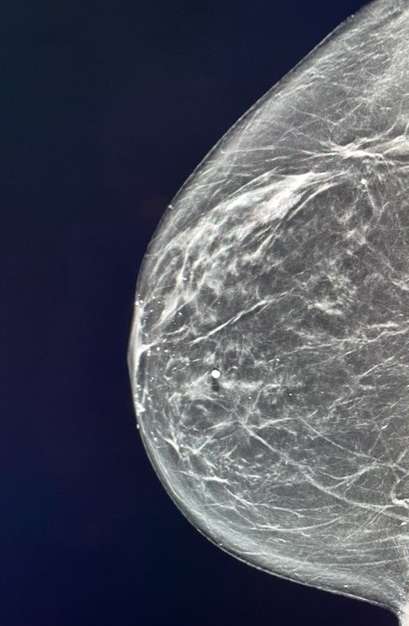
Mammography: Breast lymphomas usually present as a hyperdense solitary oval or round mass. The margins are mostly circumscribed and microlobulated, but can also be indistinct. Though asymmetry, skin thickening, and architectural distortion are quite rare imaging descriptions of lymphomas, they have been reported. Calcifications are almost always absent. Multiple small masses are suggestive of SBL.
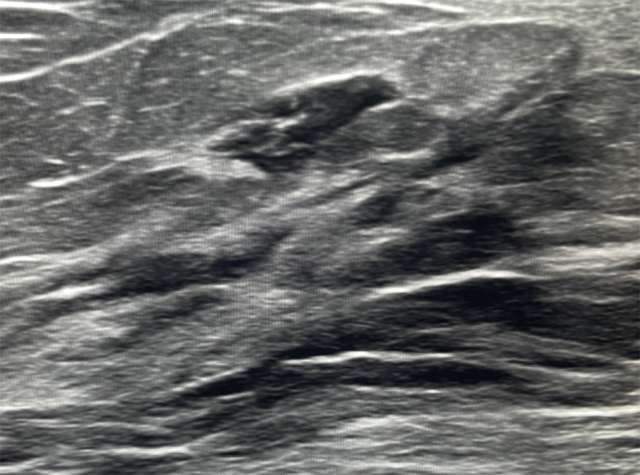
Ultrasound: Primary breast lymphoma have an unspecific appearance on ultrasound, ranging from a solitary, uncalcified, circumscribed, or indistinctly marginated mass. They are usually parallel in axis to the surrounding tissue, and are hypervascular. Posterior acoustic enhancement and echogenic rims may also be seen. SBL is usually hypoechoic or mixed echogenicity.
CT: Not a standard way of evaluating breast lymphomas, but reviews of patients with either PBL or SBL had circumscribed round or oval masses.
MRI: Typically seen as round or oval mass, with T1 hypointensity or isointensity, and areas of T2 hyperintensity. Breast lymphomas may enhance homogenously or heterogeneously, with either slow or rapid enhancement, followed by a plateau in the delayed phase. MRI is very sensitive in evaluating the presence and extent of multicentric and multifocal lesions.

PET/CT: Incredibly powerful in detecting breast lymphomas. It is both sensitive and specific in the evaluation of treatment response, tumor staging, and evaluation and/or discovery of new extranodal lymphoma.
Differential Diagnosis: As aforementioned, breast lymphoma shares radiologic and clinical characteristics with carcinoma. Therefore, fibroadenomas, phyllodes tumors, primary epithelial breast cancer, and metastases to the breast from other
Cytology/Pathology: Because breast lymphoma may have a similar imaging appearance to ductal carcinoma, pathology is an important differentiating factor in the diagnostic process. Under the microscope, lymphoma presents as noncohesive round cells of variable sizes. Lymphoma has an affinity for leukocyte common antigen, CD45, B-cells and T-cells. Because most breast lymphomas are the B-cell type, they express B-cell antigens like CD20 and have kappa or lambda light-chain restriction. The Ki-67 antigen increases in active phases of the cell cycle and can differentiate between high and low grade lymphomas. In high grade lymphoma Ki-67 proliferation rate is >40%, and low in low-grade lymphoma.
BIA-ALCL: Peri-implant effusion aspirate should be sent to cytology using a cell block prepared for multiple histologic examinations. The diagnosis is cinched with IHC staining for CD30, ALK, CD3, CD4, and CD8.
Treatment
There is no universal standard treatment of PBL or SBL. A combination of surgery, chemotherapy and radiation therapy are used. Low-grade breast lymphoma is usually treated with lumpectomy followed by radiation therapy. Research shows that mastectomy does not offer significant improvement in survival or recurrence rates. The role of radiation alone has not been shone to control breast lymphoma. Immunotherapy remains controversial. Some studies have shown improved survival in patients with advanced stage Diffuse Lymphocytic B Cell Lymphoma, though not those with breast cancer. It has not been shown to improve 5-year progression-free or overall survival rates for people with PBL.
BIA-ALCL treatment includes surgical excision of the lymphoma, the implants, as well as the surrounding fibrous capsule and any suspicious lymph nodes.
BI-RADS in Breast Lymphoma
The Breast Imaging Reporting and Data System, or BI-RADS, is a standardized system used to categorize findings in the breast. A solitary breast lesion in the setting of no known malignancy can be given a BI-RADS 4 if suspicious. Somewhat controversially, if the same solitary lesion comes back as lymphoma, and the patient has another screening mammogram showing that the finding remains, but is stable or smaller, then the patient is given a BI-RADS 2 score, with added note of known underlying disease. By the same token, bilateral axillary lymphadenopathy in the setting of known extramammary lymphoma would also be given a benign BI-RADS score, because the need to biopsy is obviated with the known malignancy.
References
- Voria P, Eby PR, Allison K. "Primary breast lymphoma." Radiol Case Rep. 2015 Nov 6;5(1):351. DOI: 10.2484/rcr.v5i1.351.
- Raj SD, Shurafa M, Shah Z, Raj KM, Fishman MDC, Dialani VM. "Primary and Secondary Breast Lymphoma: Clinical, Pathologic, and Multimodality Imaging Review." Radiographics. 2019 May-Jun;39(3):610-625. DOI: 10.1148/rg.2019180097.
- Surov A, Holzhausen HJ, Wienke A, Schmidt J, Thomssen C, Arnold D, Ruschke K, Spielmann RP. "Primary and Secondary Breast Lymphoma: Prevalence, Clinical Signs and Radiological Features." Br J Radiol. 2012 Jun;85(1014):e195-205. DOI: 10.1259/bjr/78413721.
- American College of Radiology, Breast Imaging Reporting & Data System (BI-RADS) Atlas. Mammography. Accessed on September 14, 2023.