Epilepsy
Find Your Care
Our expert neurosurgery team is committed to providing the finest and most comprehensive patient care. For help finding a neurosurgeon, call 310-825-5111.
About Epilepsy
Epilepsy is a general term covering a variety of conditions in which seizures occur. The UCLA Epilepsy Program, in affiliation with the UCLA Seizure Disorder Center, offers surgical options for treating the following types of epilepsy:
- Mesial temporal lobe epilepsy.
- Epilepsy caused by small tumors or malformations of blood vessels.
- Mesial frontal lobe epilepsy.
- Other extratemporal lobe epilepsies.
- Catastrophic epilepsy in infants and small children.
- Lennox-Gestaut syndrome or other epilepsies with drop attacks.
- Epilepsies where the seizure focus is in an area essential for function.
- Epilepsy where resection is not an option.
- Some causes of seizures include brain damage due to trauma, tumors or other brain lesions, abnormal development of the brain in early childhood, and a family history of epilepsy.
- For the majority of epilepsy patients, seizures can be fully controlled by daily medications. Antiepileptic drugs act on the brain cells to make them less likely to fire. Modern drugs continue to be developed for treating various types of seizures.
- In some patients seizures are not well controlled even after trying a number of drugs, or the medications may have side effects that are not well tolerated. Surgery should be considered in these cases.
- Patients should wait only a few years to try various epilepsy medications before evaluation for surgery. Delay results in further hardships for the patient and family, sometimes with lasting effects, especially for youngsters in school or starting their careers.
Symptoms
- During a seizure, brain cells go into a spasm of repeated firing, usually starting with a small group of cells (the seizure focus) and spreading to a larger area of the brain. Repeated seizures do not have lasting effects on the brain for the most part.
- Symptoms vary from small absence seizures, where the person is unresponsive for a few seconds or minutes, to generalized seizures, with possible falling, convulsions and repetitive behavior.
- Repeated seizures do not have lasting effects on the brain for the most part. Fortunately, nowadays the stigma of epilepsy is slowly being overcome as it is recognized that most people with epilepsy are otherwise completely normal, with intellectual and functional capabilities largely intact.
- Even so, if seizures are not controlled, the patients and their families suffer considerably because of the effects of seizures on schooling and job training, on their ability to hold a job, and on their social lives, including restrictions on driving a car and sports.
Diagnosis
- At UCLA, each patient goes through a multi-step diagnostic regimen designed to determine the best treatment option.
- Epilepsy may mean the patient is harboring a brain tumor or vascular malformation. A magnetic resonance imaging (MRI) study is recommended early on the management of epilepsy so that surgery can be performed as soon as possible if such a lesion is present.
Treatment
The location and type of damage or malformation in the brain determines the recommended epilepsy surgery option and play a critical role in treatment outcomes. Among the types of epilepsy that respond to surgery:
- Mesial temporal lobe epilepsy:
- Seizures usually start in childhood.
- In many cases the seizures originate in a small area deep in the temporal lobe on one side of the brain.
- Resection, or removal of this area, results in complete freedom from seizures in more than 70 percent of patient
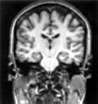
A patient with classic temporal lobe epilepsy shows a damaged right hippocampus in this MRI slice, face forward, parallel with the plane of the face. A well-formed infolding of the hippocampus is seen on the right side of the picture and only a fuzzy remnant on the left side of the picture.
- Epilepsy caused by small tumors or malformations of blood vessels:
- State-of-the-art magnetic resonance imaging (MRI) techniques reveal these lesions while still small, allowing early treatment and avoiding years of seizures and other symptoms.
- Seizures originate in the area of the lesion.
- Eighty percent of patients become seizure-free after surgical removal of the lesion and a minimum of surrounding tissue.
- Mesial frontal lobe epilepsy:
- Seizures with a motor, or movement, component indicate damage or malformation in the area of the brain that controls movement.
- Surgical treatment is difficult because traditional imaging techniques do not identify the source of the seizures.
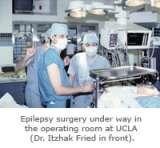
- At UCLA, doctors use electrodes to locate the seizure focus in the brain and to map essential motor function, allowing surgical removal that eliminates seizures in the majority of cases.
- Other extratemporal lobe epilepsies:
- Seizures arising in front, base and middle portions of the brain can be pinpointed, but often with more difficulty.
- The rapid spread of seizure activity in the brain means the seizures are often convulsive.
- The seizure focus may be in or near functionally important areas that should not be removed, requiring functional assessment.
- The surgical success rate, including all non-temporal surgeries but not lesions, is around 45 percent across centers in the United States.
- Catastrophic epilepsy in infants and small children:
- Seizures quickly spread over the whole brain to cause massive seizures, often severely weakening an arm or leg and slowing the child’s development.
- When the origin of the seizures can be traced to one side of the brain and a fairly large area on that side is removed, 70 percent to 80 percent of patients become seizure-free, and delayed development can be improved.
- Lennox-Gestaut syndrome or other epilepsies with drop attacks:
- A rapid spread of epileptic activity over the whole brain can cause seizures characterized by sudden loss of muscle tone that causes the patient to collapse to the ground.
- Sixty percent of patients can eliminate these drop attacks by having certain connections between the two sides of the brain severed (a corpus callosum resection), but this procedure does not control other types of seizures that may be present at the same time.
- Epilepsies where the seizure focus is in an area essential for function:
- In some cases where the seizure focus is in an area essential for communication, movement or other necessary functions, resection is not recommended.
- In rare cases surgeons will sever selected brain cell connections in the seizure focus area. Even a decrease in the number of seizures may be a relief to patients who are disabled by numerous seizures.
- Epilepsies where resection is not an option:
- Surgical placement of a vagal nerve stimulator is recommended when evaluation indicates the patient cannot be offered resection surgery, or when the patient prefers not to undergo that type of surgery.
- Acting as a type of brain cell "pacemaker," vagal nerve stimulation in some cases can curtail the increased firing of brain cells that leads to seizures.
Outcome
- The chance of becoming completely seizure-free following surgery varies according to the type of surgery.
- UCLA holds a 70 percent success rate for temporal lobe surgery, and 25 percent have noticeably fewer seizures.
- When tumors or other lesions are removed, more than 80 percent of patients become free of seizures.
- For other types of surgery the success rate is somewhat lower.
- Since extensive testing is done prior to surgery, using the most advanced imaging and brain mapping techniques, the risk of impairments due to surgery is very slim.
The Neuro-ICU cares for patients with all types of neurosurgical and neurological injuries, including stroke, brain hemorrhage, trauma and tumors. We work in close cooperation with your surgeon or medical doctor with whom you have had initial contact. Together with the surgeon or medical doctor, the Neuro-ICU attending physician and team members direct your family member's care while in the ICU. The Neuro-ICU team consists of the bedside nurses, nurse practitioners, physicians in specialty training (Fellows) and attending physicians. UCLA Neuro ICU Family Guide