Spotlight on Critical Care Anesthesiology
Spotlight on Critical Care Anesthesiology
Written by Lisa Lewis, MS

Working as a critical care physician means treating “the sickest of the sick”: patients who may have multiorgan failure and require life support machines, and who often remain hospitalized for an extended period of time.
“Frequently, people think about critical care as ‘anesthesia on steroids’ or as an extension of anesthesiology,” said Vadim Gudzenko, MD, Chief of the Critical Care Division within the UCLA Department of Anesthesiology & Perioperative Medicine (DAPM). “We do the same thing as in the operating room, but much more complex and on a bigger scale, for a longer duration of time.”
A longitudinal, multidisciplinary approach
The care that critical care anesthesiologists provide may begin in the ICU prior to surgery and then continue in the ICU postoperatively, noted Marisa Hernandez-Morgan, MD, MA, Program Director, Anesthesiology Critical Care Medicine Fellowship.
“That is one of the unique aspects of anesthesia critical care,” she said. “We’re tasked with caring for patients in and around the time of surgery, so the view that we bring, and our experience from our time in the OR, is really valuable.”
Because they are part of the intraoperative experience, anesthesiologist-intensivists “understand what the surgery entails, what the complications might be, and what to watch for in the postoperative period,” she added.
Caring for medically complex patients also means working in multidisciplinary critical-care teams, Dr. Gudzenko noted, including residents, fellows, nurse practitioners, physicians from other specialties, and ancillary support from respiratory, occupational, or physical therapists.
The Cardiothoracic ICU
About 60-70 percent of Cardiothoracic ICU patients are there following a scheduled heart surgery and generally follow a standard postoperative course, Dr. Gudzenko said, but others arrive following sudden heart failure and require extracorporeal membrane oxygenation (ECMO) or a ventricular assist device (VAD).
That in turn requires a dynamic and highly coordinated approach. “Because of the underlying disease and the machine function, there is a very complex, intricate relationship between the patient’s physiology and pathology and what the machines are doing,” Dr. Gudzenko said. “As intensivists, we need to balance all of these factors on a daily basis—frequently, we are adjusting medications and machine settings and helping the patients almost every hour.”
This requires a great deal of expertise, he noted, as well as multidisciplinary communication and coordination of care.
The Cardiothoracic ICU also includes patients who have undergone heart transplants, lung transplants, or combined organ transplantation. In the last 10 years, UCLA has seen an increase in patients receiving combined heart and liver transplants, Dr. Gudzenko said, noting that UCLA is one of the biggest centers doing these transplants in patients with congenital heart disease. “These are a unique group of patients and are probably some of the sickest patients we have.”
The Surgical ICU
As with the patients in the Cardiothoracic ICU, patients in the Surgical ICU are frequently in multiorgan failure or may be on mechanical ventilators or hemodialysis machines, but may have a wide range of postoperative or posttraumatic complications.
“Generally, we treat patients who have sustained traumatic injuries, and also patients who are about to undergo surgery or already underwent surgery and require support or management of critical illness, whether it be hemodynamic instability, bleeding complications, infectious complications, or organ failure,” said Jane Moon, MD, Associate Clinical Professor.
“We work closely with the trauma surgeons to manage patients who come through the ER, and we also work closely with surgeons from various non-cardiac surgical specialties such as Vascular Surgery, Thoracic Surgery, Surgical Oncology, Urology, ENT, and OB/Gyn,” she added.
“We manage the non-surgical issues that come up when patients have significant perioperative complications,” she said.
End-of-life considerations
Having end-of-life conversations with patients and their families is also a key part of working with critically ill patients, Dr. Gudzenko noted. “We deal with a lot of complex ethical issues,” he said, “which puts us at the crossroads of medicine, ethics, and palliative care.”
Dr. Gudzenko and critical care anesthesiologist Brannon Altenhofen, MD, have worked together over the last few years to ensure that palliative care specialists are involved early on, when patients are first placed on life support machines.
The goal, Dr. Altenhofen said, was “establishing the expectation of having these conversations about values and family involvement, and setting expectations for what recovery may or may not look like early on in the hospitalization, rather than waiting until it became clearer that we were approaching end-of-life.”
“That transition of care is a challenging one for both the clinicians and the family,” Dr. Altenhofen said, “but it’s a really important part of what we do.”
As Dr. Moon noted, “It’s an honor to be able to care for patients during their most vulnerable periods. It’s rewarding to see patients who are extremely sick get better, but also to help patients and families navigate uncertainty and times when the outcomes may be less desirable.”
Critical care initiatives and research
On an ongoing basis, the physicians in the Critical Care Division are focused on designing and implementing new programs to continue to improve patient outcomes.
Improving sudden-cardiac-arrest outcomes

One such program, piloted in conjunction with Los Angeles County Emergency Management Services, has changed initial treatment for patients with sudden cardiac arrest in the field.
“Together with our cardiac surgeons, our intensivist group was one of the driving forces for this,” Dr. Gudzenko said. He and Peyman Benharash, MD, Director of Adult ECMO Services, were the trial leads from UCLA.
During the pilot, which ran from 2020 through 2022, Ronald Reagan UCLA Medical Center was one of three participating centers designated as capable of providing eCPR (via ECMO) for patients experiencing out-of-hospital cardiac arrest. Compared to patients treated in the field with conventional resuscitation, the survival rate for patients transported to one of the three ECMO centers more than doubled. As a result, the protocol has been expanded to additional centers and will continue to be rolled out further as a new standard of care.
“Essentially, we changed the system of providing care to patients with out-of-hospital cardiac arrest in L.A. County,” Dr. Gudzenko said.
Recognition from the American Heart Association
As Co-Medical Director of the “Code Blue” response team at Ronald Reagan UCLA Medical Center, critical care anesthesiologist Andrew “Ace” Young, MD, reviews every in-hospital cardiac arrest. In this role, he also determines any improvements to the hospital’s “Code Blue” policy that may be needed.
Dr. Young noted that last year marked a first for the hospital: a “Get With the Guidelines” Silver Award from the American Heart Association as a recognition of excellence in meeting the most up-to-date guidelines for resuscitation.
Ambient AI scribe technology
Looking ahead to 2026, the Critical Care Division will soon be piloting the first in-patient use of ambient AI scribe technology at UCLA, using generative AI to create a comprehensive summary of ICU rounds. The pilot is being jointly spearheaded by Laleh Jalilian, MD, Physician Informaticist, and co-investigator Matthew “Scott” Vandiver, MD, PhD, Associate Program Director, Anesthesiology Critical Care Medicine Fellowship. The trial will use the same technology that is already being used in the outpatient setting, Dr. Vandiver noted.
Decreasing delirium

Another initiative expected to start in early 2026 will focus on reorienting patients in the Cardiothoracic ICU via pre-recorded video messages from their families. The videos will be similar to those recorded during Covid as alternatives to in-person visits.
Dr. Vandiver and Brionna “Brie” Bulgarelli, MD, anesthesiology resident physician, hope that the videos will help decrease delirium, particularly among elderly patients. “Family members have a much better rate of reorienting patients,” Dr Vandiver noted. “Having a family member tell them ‘You’re in the hospital because you just had heart surgery, you’re OK, we love you, the nurses are there to help you,’ can really improve patient care.”
Additional research
Among other projects, Dr. Vandiver is currently the principal investigator for a study evaluating a new protocol for treating patients with acute kidney injury (AKI) who are receiving continuous renal replacement therapy. Known as the Neutralize AKI trial, the trial adds a specialized filter, in addition to the dialysis filter, to remove highly activated neutrophils (a type of white blood cell). “These are highly activated immune cells,” Dr. Vandiver said. “The thinking is that the immune system is so revved up that it’s actually harming the patient.”
Training and professional development
A strong fellowship program

Both Dr. Hernandez-Morgan, Program Director, and Dr. Vandiver, Associate Program Director, are continuing to strengthen the Anesthesiology Critical Care Medicine Fellowship program, expanding the didactic curriculum and encouraging fellows to conduct research and present at professional conferences.
“We have the support of the entire ICU division,” Dr. Hernandez-Morgan said, “and I think that really makes the fellowship so strong.”
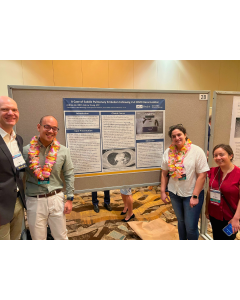
All of the recent fellows have presented at the Society of Critical Care Anesthesiologists (SOCCA) Annual Meeting. Last year, Emma Huebner, MD, received a Young Investigator Award for a project she worked on with Dr. Vandiver focusing on brain changes in heart transplant patients.
Fellows have also presented at both the International Society for Heart and Lung Transplantation and at EuroELSO (the European Chapter of the Extracorporeal Life Support Organization).
In addition to the anesthesiology critical care fellows, the Cardiothoracic ICU and Surgical ICU rotations also host outside fellows from Cardiology and Pulmonology and Critical Care Medicine, noted Joseph Meltzer, MD, Medical Director of the Cardiothoracic ICU.
Expanding bedside ultrasound training
Given that intensivists are frequently called upon to conduct bedside ultrasounds, the department launched an educational workshop series in 2025 to provide hands-on training.
The initial cohort included a cross-section of 12 anesthesiologists, said Dr. Altenhofen, who worked with Sumit Singh, MD, Director of the Surgical ICU at the Greater Los Angeles VA Hospital, and Judi Turner, MD, PhD, DAPM Vice Chair for Education, to design the curriculum. He and Dr. Singh jointly led the workshops, with assistance from Dr. Vandiver and from David Boldt, MD, Division Chief, Trauma and Adult Multi Specialty Anesthesia; Rana Movahedi, MD, Director of the Regional Anesthesiology and Acute Pain Medicine Fellowship; and George Lim, MD, critical care intensivist and emergency medicine physician.
“There’s been a lot of enthusiasm in the department,” Dr. Altenhofen said, noting that the initial waitlist was more than 50 people. The second cohort will be selected in January 2026 and will begin later in the spring.
Providing help wherever it’s needed
Dr. Meltzer, who served as the inaugural Chief of Critical Care Anesthesiology at UCLA when the subspecialty was formed in 2012, has seen it grow into one of the larger ones within the department.
“Our division also happens to be multidisciplinary,” he said, “with surgeons, emergency medicine physicians, and anesthesiologists, all of whom are subspecialty trained in critical care medicine.”
The group also provides in-house, on-call services around the clock. “Because we keep an attending in-house all the time, we not only tend to the patients on our service,” he said, “but also provide hospital-wide procedural and medical support and supervision for patients who may be vulnerable or in extremis.”
As Dr. Gudzenko noted, “We are the highest level of ICU providers who are in-house. With our patient population, we need to have the highest level of expertise available, immediately.”
The intensivists who are on call respond to emergencies throughout the hospital and in the operating room whenever there’s a need for additional support or expertise, Dr. Vandiver noted, characterizing the on-call service as “an impressive collaboration.”
As he summed up, “It’s great for the patient, and it helps take some of the load off the operating room staff,” he said. “It’s also great for when the patient transitions to the ICU, because we’ve already seen them in the operating room and know what’s going on, so we can take better care of them.”