Case: Inflammatory Breast Cancer
by Shannon Yoo, MD and Reza Fardanesh, MD
Clinical Presentation
Patients present with rapid onset (typically less than 3 months) of asymmetric breast enlargement accompanied by tissue thickening, erythema, induration, and warmth involving greater than one third of the breast tissue. The pathognomonic finding is dimpling of the skin known as peau d'orange, which occurs due to obstruction of the dermal lymphatics by the tumor emboli. In general, the clinical symptoms mimic mastitis; however, inflammatory breast cancers will not respond to 1-2 week trials of antibiotics treatment. A palpable breast mass is present in approximately 50% of the cases. There may be presence of unilateral fixed and palpable lymph nodes. Due to the aggressive nature of the disease, patients typically present at an advanced stage with distant metastases, which is present in upwards of 20-40% of cases at the initial presentation.
Epidemiology
Inflammatory breast cancer accounts for approximately 1-3% of all breast cancers. An average age at diagnosis ranges between 55-58 years. It is seen almost exclusively in females.
Pathology
In general, invasive ductal carcinoma is more common compared to invasive lobular carcinoma. Invasion of the dermal lymphatics by tumor cells is pathognomonic for inflammatory breast cancer but is not necessary to clinch the diagnosis. With the invasion of dermal lymphatics, the TNM stage is T4d with anatomic stage of III.
Radiographic Features
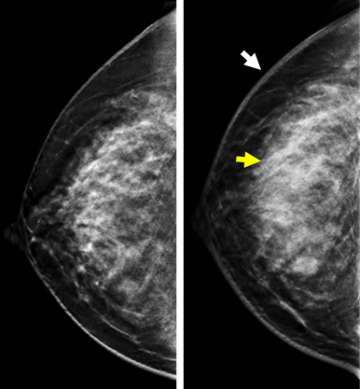
Mammography/ DBT
Typical mammographic findings include global or focal asymmetry, skin thickening, trabecular thickening, diffuse increase in breast density, and stromal coarsening (Figure 1). In addition, dense and irregular axillary adenopathy are seen in approximately one half of the cases. Multiple masses and pleomorphic calcifications are uncommonly described features.
Ultrasound
The most common features are asymmetric skin thickening and subcutaneous edema. Diffuse, multifocal, irregular, hypoechoic, and shadowing masses that are mammographically-occult may be seen. Dermal lymphatic invasion manifests as multiple small anechoic spaces within the dermis.
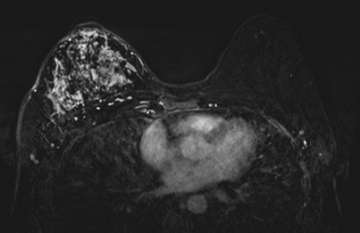
MRI
The most common imaging features of IBC are diffuse skin thickening and edema. Extensive or segmental non mass-like enhancements are commonly seen (Figure 2). MRI can accurately detect a primary breast lesion in 98-100% of cases, which is superior to mammography or ultrasound. Diffusion-restricting irregular and spiculated mass or masses can be seen with rapid enhancement and delayed or plateau washout characteristics. Thickened skin may also exhibit diffusion restriction and focal enhancement. Tumor emboli in the lymphatic spaces may manifest as reticular/dendritic enhancement. MRI is the best imaging modality to accurately predict local treatment response based on the size of the tumor per Response Evaluation Criteria in Solid Tumors 1.1 criteria. MRI is also useful in assessing the extent of extraparenchymal involvement, including local chest wall invasion as well as lymphadenopathy.
FDG-18 PET/CT
Given the aggressive nature of the disease, PET/CT is useful in initial evaluation and in staging to determine the extent of lymph node involvement and to detect distant metastasis. It is superior to radionucleotide bone scan in assessment of the osseous metastasis. It is also useful in determining local and metastatic treatment response, with greater than 50% decline in FDG uptake characterized as good response and less than 50% decline in FDG uptake characterized as non-responding tumor.
Biopsy
Skin punch biopsy may yield diagnostic results in up to approximately 75% of patients, where tumor emboli in dermal lymphatics may be seen in pathology specimens. Ultrasound-guided core biopsy of a mass is the standard of care. Ultrasound-guided biopsy of the axillary node is used for staging of regional nodes prior to neoadjuvant chemotherapy. Both the tissue diagnosis and clinical presentation are required for diagnosis.
Treatment and prognosis
Patients that have undergone all 3 treatment modalities, including neoadjuvant chemotherapy, modified radical mastectomy, and radiation therapy have improved outcomes. Neoadjuvant chemotherapy is the mainstay of initial treatment as surgery is contraindicated due to the diffuse skin involvement at initial presentation. Modified radical mastectomy and axillary lymph node dissection is the second form of care for patients with stage III IBC. In absence of metastatic disease, chest wall radiation therapy is a standard of care for all patients after mastectomy. The 2 year survival rate is approximately 84%.
References
- Robertson FM, Bondy M, Yang W, Yamauchi H, Wiggins S, Kamrudin S, Krishnamurthy S, Le‐Petross H, Bidaut L, Player AN, Barsky SH. "Inflammatory Breast Cancer: The Disease, the Biology, the Treatment." CA Cancer J Clin. 2010 Nov-Dec;60(6):351-75. DOI: 10.3322/caac.20082.
- Yeh ED, Jacene HA, Bellon JR, Nakhlis F, Birdwell RL, Georgian-Smith D, Giess CS, Hirshfield-Bartek J, Overmoyer B, Van den Abbeele AD. "What Radiologists Need to Know About Diagnosis and Treatment of Inflammatory Breast Cancer: A Multidisciplinary Approach." Radiographics. 2013 Nov-Dec;33(7):2003-17. DOI: 10.1148/rg.337135503.
- Leung, Jessica. "Inflammatory Breast Carcinoma." STATdx
- "Inflammatory Breast Carcinoma." RADPrimer