Case: Skin Lesion
by Marie Cumigad, MD and Reza Fardanesh, MD
Skin lesions are common imaging findings in the breast. It is important to distinguish between skin lesions and superficial breast lesions. Lesions arising from the skin layer are often benign while lesions arising from the superficial subcutaneous fat or breast parenchyma has a relative higher chance of being cancer. Superficial breast lesions require radiologic imaging workup whereas skin lesions require a dermatologic consultation. A thorough understanding of anatomy, as well as various localization techniques from each modality are used to differentiate one from the other.
Anatomy
The dermis is subdivided into three layers: the epidermis, dermis and hypodermis/ subcutaneous fat layer. The epidermis is very thin with thickness measuring 0.5-2 mm made up of several layers of keratinocytes, making it indistinguishable as a separate layer on imaging (1). The dermis is composed of hair follicles, nerve endings, blood vessels, lymphatics and fatty tissue.
The breast is functionally considered as a modified apocrine gland for milk production in breast feeding. The breast is composed of mammary glands consisting of fibrous, glandular and adipose tissue, organized into 15-20 lobes arranged in a radial pattern around the nipple. Milk production starts with the terminal duct lobular unit, the basic functional unit of the breast. The terminal duct lobular unit is also the where malignant and benign lesions primarily arise from. Cooper’s ligaments are suspensory ligaments that functions as structural support in the breast tissue. This structure extends through the subcutaneous fat and affix the underlying breast with the skin through its superficial extensions known as retinacula cutis (2). Terminal duct lobular unit may extend into the Copper’s ligaments which may be located in the subcutaneous fat, hence a potential location for superficial breast cancers.
Localization Techniques
Aside from masses and architectural distortion, mammography is most useful for detecting breast calcifications. When calcifications project near the surface of the skin, dermal location must be considered and further worked up. The tangential view is used to prove the dermal location of a lesion by obtaining an image of the area of interest in tangent to the x-ray beam bringing into view the skin surface and the contrasting subdermal fatty tissue. The area of interest is localized with a skin BB marker through an alphanumeric grid guide. An imaginary line is then drawn from the BB marker towards the nipple. The tangential view is then obtained by rotating the C-arm so that the image receptor is parallel to the imaginary line.
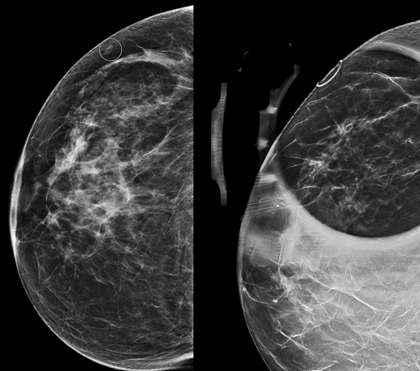
Tomosynthesis can also be used for demonstrating dermal location of a lesion. In tomosynthesis, images obtained from multiple angles of a stationary compressed breast are reconstructed into series of thin 1-3 mm slices that span from the compression paddle to the beam detector (3). Skin lesions can then be identified by the superficial location of the reconstructed slice on which they are in focus.
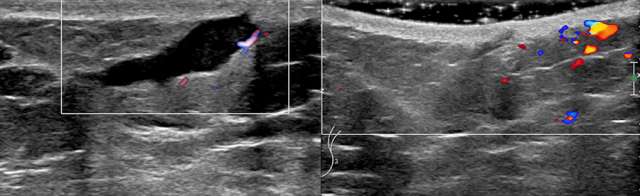
Ultrasound is the imaging modality of choice for solid masses as the superior spatial resolution allows for optimal definition of skin layers. On ultrasound, the dermal layer appears as a hyperechoic band overlying the relatively more hypoechoic subcutaneous fatty tissue. Lesions completely bordered within this echogenic dermal layer can be confidently considered dermal in origin. Dermal lesions can extend to the subcutaneous layer which may be difficult to distinguish from breast tissue origin. Sonographic features such as the “claw sign” and “tract-to-skin sign” are strongly suggestive of dermal origin (4). Another tool that improves spatial resolution of ultrasound is through the use of acoustic gel.
MRI has been utilized for the assessment of epidermal/dermal abnormalities, such as neurofibromas, hemangiomas, or epidermal inclusion cysts (5). Due to its lesser spatial resolution than ultrasound, it is less accurate in terms of skin lesion localization. Skin cysts are often T1- hypointense and T2-hyperintense lesions. It may occasionally show peripheral rim enhancement or internal enhancement.
References:
- Fornage BD. "Sonography of the Skin and Subcutaneous Tissues." Radiol Med. 1993 May;85(5 Suppl 1):149-55. PMID: 8332789.
- Kopans D. "Anatomy, Histology, Physiology, and Pathology." Breast Imaging. 2nd ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 1998; pp. 3-27.
- Friedewald SM. "Breast Tomosynthesis: Practical Considerations." Radiol Clin North Am. 2017; 55(3):493-502. DOI: 10.1016/j.rcl.2016.12.004.
- Stavros AT. "Breast Anatomy: The Basis for Understanding Sonography." Breast Ultrasound. Philadelphia, Pa: Lippincott Williams & Wilkins, 2004; pp. 56-108.
- Beaman FD, Kransdorf MJ, Andrews TR, Murphey MD, Arcara LK, Keeling JH. "Superficial Soft-tissue Masses: Analysis, Diagnosis, and Differential Considerations." Radiographics. 2007 Mar-Apr;27(2):509-23. DOI: 10.1148/rg.272065082.